Billing in orthopedics isn’t just about submitting claims; it’s about making sure every procedure, diagnosis, and modifier is coded correctly so your practice gets paid on time and stays compliant. If you’ve ever felt overwhelmed by complex CPT codes, confusing ICD-10 updates, or repeated claim denials, you’re not alone. Orthopedic billing requires a unique skill set because it covers everything from fracture care and joint replacements to injections, braces, and surgical procedures.
The good news? With the right orthopedic billing guidelines, you can streamline your workflow, reduce costly errors, and protect your revenue cycle. In this article, we’ll explore CPT and ICD-10 codes, modifiers, payer-specific rules, compliance tips, and documentation best practices, so you can focus more on patient care and less on billing headaches.
What is Orthopedic Billing and Why is it Important?
Orthopedic billing is a specialized branch of medical billing that focuses on claims for orthopedic services such as fracture care, joint replacements, arthroscopies, injections, and spinal treatments. Unlike general billing, orthopedic billing requires detailed knowledge of surgical procedures, postoperative care, and the correct use of modifiers.
The importance of accurate orthopedic billing cannot be overstated. It ensures proper reimbursement, minimizes claim denials, and protects practices from compliance risks.
A small mistake in coding or modifier usage can lead to significant revenue loss, which is why orthopedic practices need to follow structured billing guidelines.
Essential Orthopedic Billing Guidelines
CPT Codes Frequently Used in Orthopedics
CPT codes form the foundation of orthopedic billing. Using the wrong code or missing one can result in rejected claims. Below are some of the most common orthopedic CPT codes:
- Fracture Care Codes: 27236 (Hip fracture), 23500 (Clavicle fracture), 27750 (Ankle fracture)
- Joint Replacement Codes: 27130 (Total hip arthroplasty), 27447 (Total knee arthroplasty)
- Injection and Pain Management Codes: 20610 (Joint injection), 62321 (Epidural injection)
- Arthroscopy Codes: 29881 (Knee arthroscopy), 29880 (Meniscectomy)
Understanding and applying these codes correctly improves claim accuracy and reduces delays.
ICD-10 Codes in Orthopedic Billing
ICD-10 coding requires precision. Orthopedic conditions are often specific to body parts, laterality, and the nature of injury. Here are examples of commonly used ICD-10 codes:
- Fractures: S72.001A (Fracture of unspecified part of neck of right femur)
- Joint Conditions: M16.0 (Osteoarthritis of the hip), M17.11 (Unilateral primary osteoarthritis, right knee)
- Sports Injuries: S83.511A (ACL tear, right knee)
- Spinal Conditions: M48.0 – Other Spondylopathies (M48.06 – Spinal Stenosis, lumbar region. M48.061 – Spinal Stenosis lumbar region without neurogenic claudication. M48.062 – Spinal stenosis, lumbar region with neurogenic claudication)
Accuracy in ICD-10 coding links the diagnosis to the procedure, which is critical for proving medical necessity and avoiding denials.
HCPCS Codes for Orthopedic Supplies and Services
Orthopedic care often involves braces, splints, casting materials, and durable medical equipment. These require HCPCS codes for reimbursement:
- Braces and Splints: L1833 (Knee orthosis)
- Casting and Strapping: Q4010 (Cast supplies, short arm fiberglass)
- Durable Medical Equipment: E0110 (Crutches)
Using the right HCPCS codes ensures practices are paid for both the service and the necessary supplies.
Common Orthopedic Billing Modifiers
Modifiers in orthopedic billing help clarify procedures and prevent duplicate claim issues. Below are some of the most used modifiers:
- Modifier 25: Significant E and M service performed on the same day as a procedure
- Modifier 50: Bilateral procedure
- Modifier 59: Distinct procedural service
- Modifier 76 and 77: Repeat procedure by the same or different physician
- Modifier 80 and 82: Assistant surgeon involvement
- Modifier LT and RT: Identifying left or right side procedures
Correct use of modifiers provides insurers with a complete picture of the services performed and ensures fair payment.
Documentation Best Practices for Orthopedic Billing
Strong documentation is the backbone of orthopedic billing. Without proper documentation, even correctly coded claims can be denied. Practices should focus on the following:
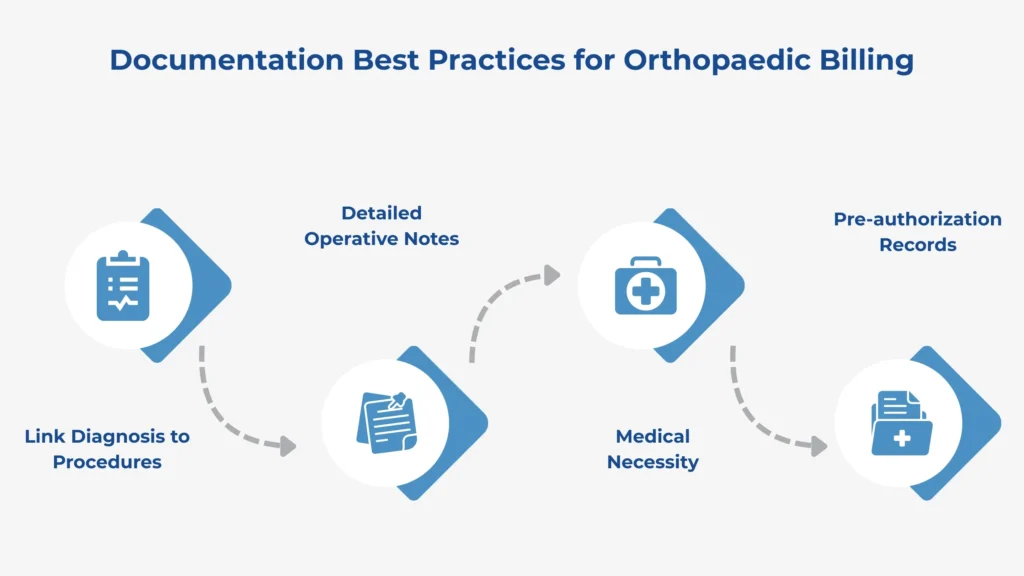
- Link Diagnosis to Procedures: Each procedure must be tied to a diagnosis that justifies medical necessity.
- Detailed Operative Notes: Surgical reports should describe the procedure in detail, including laterality and the extent of the service.
- Medical Necessity: Always document why the procedure or service was needed.
- Pre-authorization Records: For high-value procedures such as joint replacements or spinal surgeries, pre-authorization is often required. Keeping this on file avoids payer disputes.
Insurance and Payer-Specific Rules in Orthopedic Billing
Every insurance provider has its own set of requirements for orthopedic claims. Understanding these payer rules can save practices time and money.
Medicare Orthopedic Billing: Medicare follows strict guidelines regarding global periods, bundled services, and modifier use. For example, postoperative visits within the global period are not separately billable unless they are unrelated to the surgery.
Commercial Payers: Private insurers such as Aetna, BlueCross, and UnitedHealthcare may have different prior authorization requirements and reimbursement rates. Some payers require documentation of failed conservative treatments before approving surgeries.
Workers’ Compensation Claims: Orthopedic injuries are common in workplace accidents. Workers’ compensation has unique reporting requirements and often requires additional documentation, such as employer injury reports and detailed operative notes.
Orthopedic Global Billing Guidelines
The global surgical package is an important concept in orthopedic billing. It refers to all services that are considered part of a surgical procedure and are not separately billable.
- Pre Operative Care: Office visits prior to surgery that are related to the procedure are bundled into the global payment.
- Post Operative Care: Routine follow-up visits, wound checks, and suture removals during the global period are included in the original payment.
- Unrelated Services: If a patient comes back for a condition that is unrelated to the surgery, that visit can be billed separately with the right modifier.
Understanding these rules prevents unintentional duplicate billing and helps avoid compliance risks.
Common Orthopedic Billing Errors and Denials
Orthopedic billing is complex, and errors are common. Here are some of the top mistakes practices make:
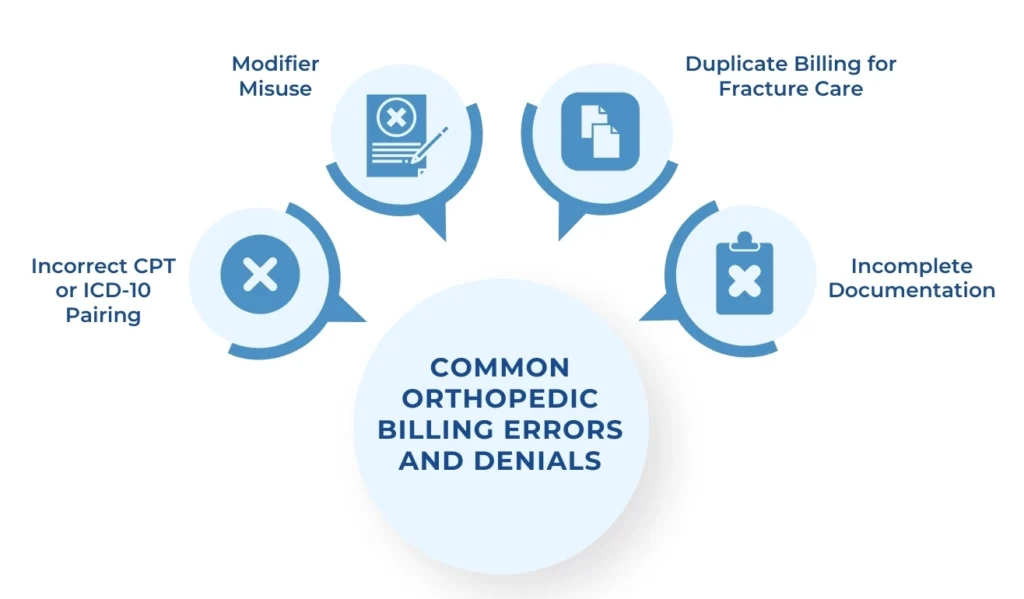
- Incorrect CPT or ICD-10 Pairing: When the diagnosis does not justify the procedure, claims are denied.
- Modifier Misuse: Applying modifier 25 or 59 incorrectly can trigger audits.
- Duplicate Billing for Fracture Care: Fracture care includes both the initial treatment and follow-ups within the global period. Billing separately often leads to denials.
- Incomplete Documentation: Missing operative notes, pre-authorizations, or medical necessity statements can delay reimbursement.
Compliance in Orthopedic Billing
Compliance is not optional in orthopedic billing. With strict CMS and HIPAA regulations, practices must ensure that claims are accurate and ethical.
- CMS Guidelines: Providers must follow coding edits such as NCCI edits, which prevent unbundling of services.
- HIPAA Regulations: Patient data must be kept secure when submitting electronic claims.
- Fraud and Abuse Prevention: Upcoding, unbundling, and billing for services not performed can result in severe penalties. Following compliance protocols protects both the practice and its patients.
Role of Technology in Orthopedic Billing
Modern technology can make orthopedic billing less stressful and more accurate.
- EHR and Practice Management Systems: These systems streamline coding, documentation, and claim submission.
- AI-Based Claim Scrubbing Tools: Automated systems can flag errors before claims are submitted, reducing denials.
- Outsourcing Orthopedic Billing: Partnering with professional billing services can help practices focus on patient care while experts handle the complexities of coding, compliance, and collections.
Orthopedic Billing Checklist
A quick checklist can help practices reduce errors and improve claim acceptance rates:
- Confirm patient insurance coverage
- Obtain prior authorizations when required
- Use accurate CPT, ICD-10, and HCPCS codes
- Apply modifiers correctly
- Document medical necessity
- Submit claims electronically for faster processing
- Track claim status and follow up promptly
Closing Note
Orthopedic billing is detailed, complex, and often overwhelming, but following the right guidelines can simplify the process. By mastering CPT, ICD-10, and HCPCS coding, applying modifiers correctly, maintaining accurate documentation, and understanding payer rules, practices can significantly reduce denials and improve cash flow.With the right combination of technology, compliance, and expertise, orthopedic billing can move from a constant headache to a streamlined process that supports both providers and patients. If your practice is struggling with orthopedic billing, consider partnering with a professional orthopedic medical billing service from RevenueES to maximize efficiency and revenue.