In the world of medical billing, accuracy isn’t just important, it’s everything. Submitting the wrong type of claim can delay payment, trigger rejections, or even lead to compliance risks. That’s why understanding the difference between institutional claims and professional claims is essential for healthcare providers, billing specialists, and revenue cycle managers alike.
Whether you’ve heard these terms as professional vs institutional claims, facility vs professional billing, or even medical claims vs hospital claims, the core idea remains the same: each claim type serves a distinct purpose, uses specific forms, and follows different payment rules.
In this article, we’ll break down each type in detail, compare UB-04 vs CMS-1500, clarify 837i vs 837p, and answer the most common questions so you can bill with confidence and get paid faster.
What Are Institutional Claims?
Institutional claims are used to bill for facility-based services provided in hospitals, nursing facilities, rehab centers, and similar institutional settings. These claims are typically submitted by the institution itself, rather than an individual provider, and are designed to capture the costs of resources, equipment, and overhead associated with patient care.
Institutional claims are submitted on the UB-04 form (also known as CMS-1450) and often include services like:
- Inpatient hospital stays
- Outpatient hospital services
- Laboratory tests performed in a hospital
- Skilled nursing facility care
- Home health agency services
Unlike professional claims, institutional billing often uses Diagnosis-Related Groups (DRGs) or Ambulatory Payment Classifications (APCs) to determine payment amounts. This makes it a facility-focused process rather than one centered on individual provider work.
Example:
A patient undergoes knee replacement surgery in a hospital. The hospital will submit an institutional claim for the operating room, nursing care, anesthesia equipment, recovery room, and any other facility-based costs.
What Are Professional Claims?
Professional claims represent the billing for individual healthcare providers’ professional services, think doctors, nurse practitioners, physician assistants, therapists, and other licensed clinicians. These are person-focused claims, capturing the expertise and labor of the provider rather than the facility’s resources.
Professional claims are billed using the CMS-1500 form, which records the provider’s NPI (National Provider Identifier), service codes, and patient encounter details. Payment is usually determined by CPT (Current Procedural Terminology) or HCPCS (Healthcare Common Procedure Coding System) codes, each with its own fee schedule.
Example:
In the same knee replacement scenario, the orthopedic surgeon who performs the surgery will submit a professional claim for their surgical work, while the anesthesiologist will submit another professional claim for anesthesia administration.
Institutional Billing vs. Professional Billing
While both institutional and professional billing ultimately aim to secure payment for healthcare services, their processes, forms, and reimbursement structures differ in key ways:
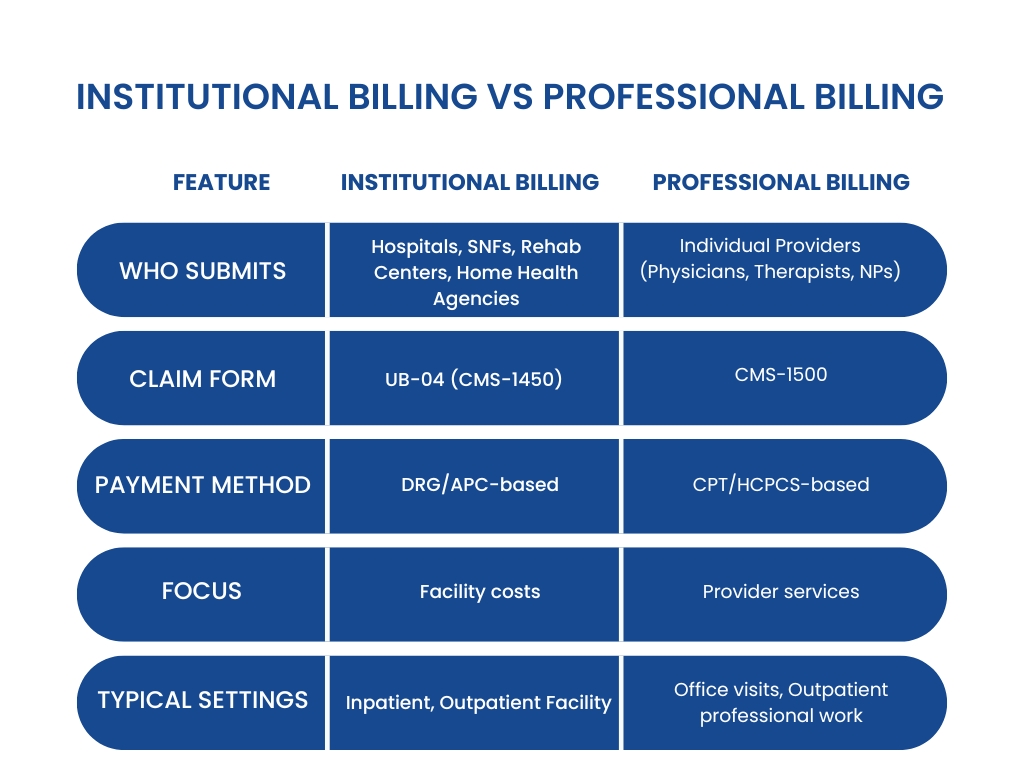
In short, Institutional billing vs professional billing comes down to facility vs provider, UB-04 vs CMS-1500, and grouped payment vs fee-for-service models.
UB-04 vs CMS-1500: Understanding the Claim Forms
UB-04 (CMS-1450)
- Used by institutions such as hospitals, SNFs, and rehab centers.
- Captures facility-level services like room charges, nursing care, and facility equipment use.
- Requires revenue codes, type of bill codes, and condition codes.
CMS-1500 (HCFA 1500)
- Used by individual healthcare providers to bill for professional services.
- Captures details like provider NPI, CPT/HCPCS codes, and modifiers.
- Often used by outpatient clinics and physician offices.
Difference Between UB-04 and CMS-1500
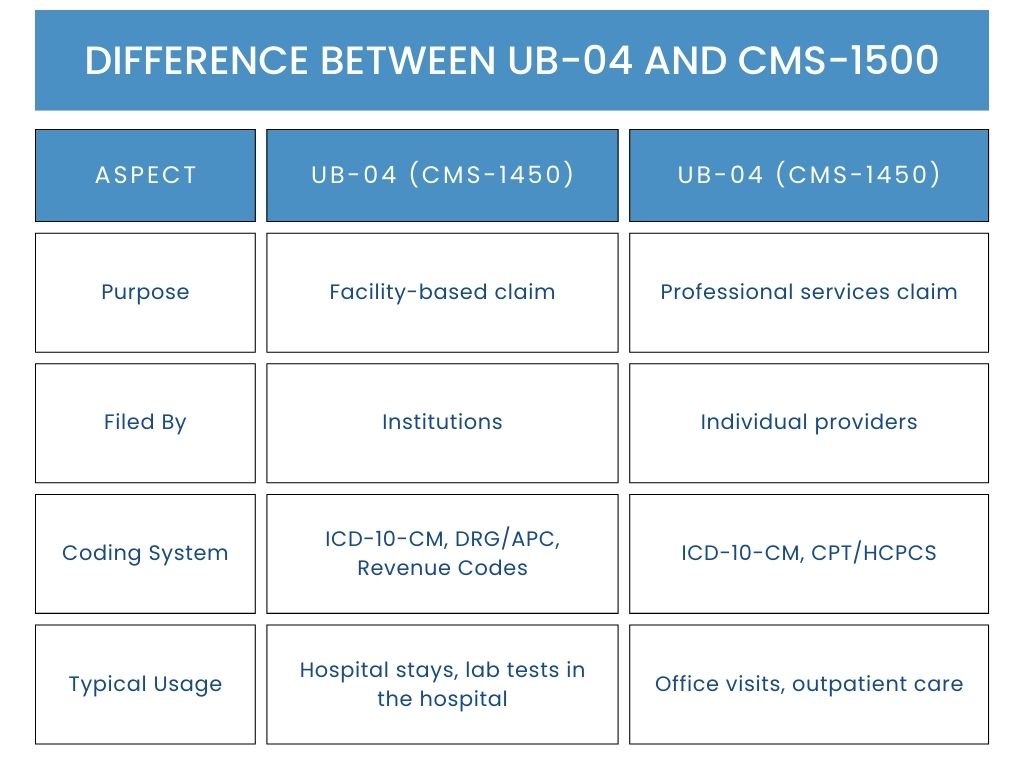
In practice:
If you’re wondering what would usually get billed on the UB-04 vs the CMS-1500 form? Remember this simple rule:
- UB-04 → Facility and hospital services.
- CMS-1500 → Professional and provider services.
837i vs 837p: The Electronic Claim Formats
With electronic billing becoming the norm, both institutional and professional claims have their digital counterparts:
- 837i: The electronic format for institutional claims (think “i” for institution). Mirrors the UB-04 form in an EDI (Electronic Data Interchange) format.
- 837p: The electronic format for professional claims (think “p” for professional). Mirrors the CMS-1500 form.
Both formats are HIPAA-compliant and are required by most payers for claim submission, with only rare exceptions for paper claims.
Medical Claims vs Hospital Claims
The terms medical claims and hospital claims are often used interchangeably, but they aren’t identical.
- Medical claims: A broad term referring to any request for payment submitted to an insurer for healthcare services, which includes both institutional and professional claims.
- Hospital claims: A more specific subset of medical claims that applies only to hospital-based services. These are institutional claims submitted on a UB-04 form or electronically via 837i.
Example:
- A claim for a physical therapy session in a private clinic → Medical claim (professional claim).
- A claim for an inpatient stay in a hospital → Hospital claim (institutional claim).
Understanding this distinction helps avoid confusion when reading payer rules and compliance requirements.
Professional vs Facility Claims: Payment and Processing Differences
While both types ultimately result in reimbursement, how they are paid is very different:
Professional Claims (CMS-1500 / 837p)
- Payment is typically fee-for-service, based on CPT/HCPCS codes.
- Each service or procedure is priced individually according to the payer’s fee schedule.
- Reimbursement goes directly to the provider or their practice.
Facility Claims (UB-04 / 837i)
- Payment is often bundled through DRG (Diagnosis-Related Group) for inpatient services or APC (Ambulatory Payment Classification) for outpatient services.
- This bundled rate covers a range of facility costs.
- Reimbursement goes to the facility, not the individual provider.
Key takeaway:
Professional vs facility billing is really a matter of service-level detail vs bundled facility cost, and this affects both coding and payment strategy.
Common Mistakes When Submitting Institutional or Professional Claims
Submitting the wrong type of claim can result in denials, payment delays, or even compliance issues. Common pitfalls include:
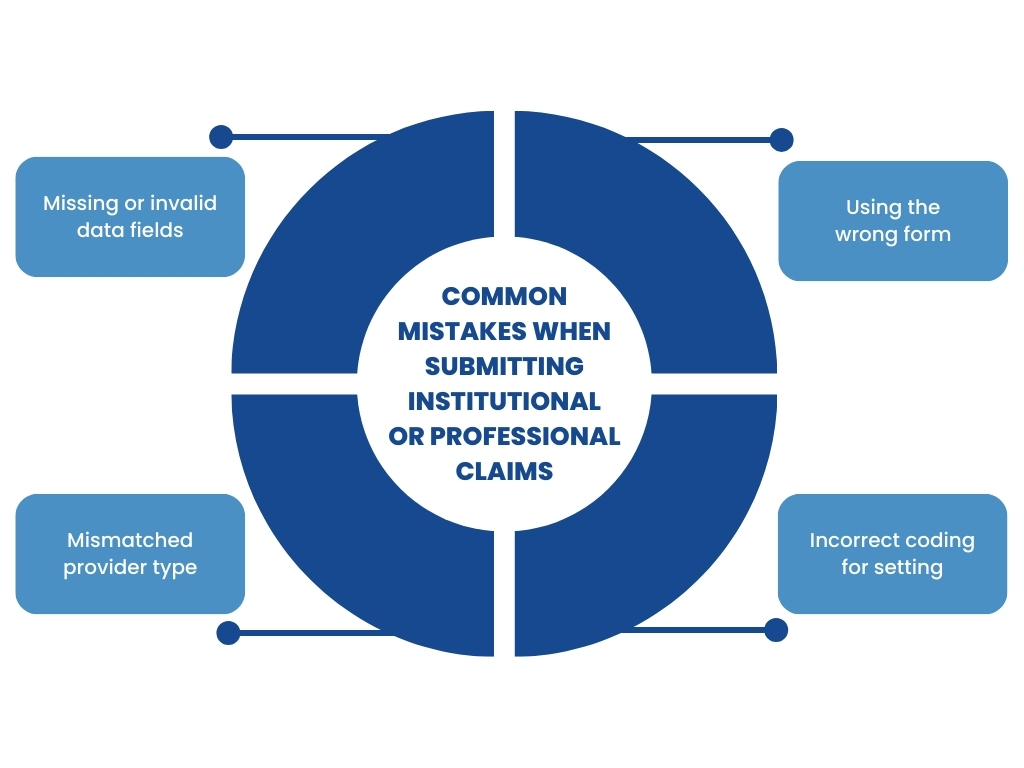
- Using the wrong form: Submitting a hospital stay on a CMS-1500 instead of a UB-04.
- Incorrect coding for setting: Using professional CPT codes in an institutional claim without proper revenue codes.
- Mismatched provider type: Listing a facility as the billing provider on a CMS-1500 or vice versa.
- Missing or invalid data fields: Incomplete NPI, incorrect diagnosis codes, or missing modifiers.
Best Practices for Accurate Medical Billing
To avoid errors and maximize timely payments:
- Verify the provider and setting type before choosing the claim form.
- Use correct coding systems for the claim type (CPT/HCPCS for professional, DRG/APC for institutional).
- Stay updated on CMS and payer guidelines for form use.
- Train billing staff to recognize the difference between institutional billing and professional billing workflows.
The Bottom Line
Correctly handling professional vs institutional claims isn’t just about paperwork; it’s about protecting your revenue, ensuring compliance, and building a reliable billing workflow. Whether you’re navigating professional vs facility claims, dealing with the complexities of institutional billing vs professional billing, or just trying to figure out what gets billed on the UB-04 vs the CMS-1500, having the right expertise makes all the difference.
At RevenueES, we specialize in helping healthcare providers, facilities, and billing teams streamline claims submission, reduce denials, and get paid faster. From medical claims vs hospital claims to professional vs facility billing, we know the rules, forms, and coding systems inside out, so you don’t have to.