Healthcare providers are under constant pressure to balance quality of care, patient satisfaction, and financial sustainability. Traditional reimbursement methods like fee-for-service (FFS) reward volume rather than value, often leading to inefficiencies, unnecessary procedures, and unpredictable revenue streams. To address these challenges, many health systems and payers have shifted toward value-based payment models, and one of the most widely adopted approaches is capitation.
But what exactly is capitation? How does it differ from other models like bundled payments or FFS, and what risks and benefits does it bring for providers? Let’s explore it!
What is Capitation in Medical Billing?
At its core, capitation in medical billing is a payment arrangement where healthcare providers receive a fixed, upfront amount per patient, per month (PMPM), regardless of how many services a patient uses during that period. This model shifts financial responsibility to the provider, encouraging efficiency and preventive care.
Instead of billing for every test, procedure, or appointment, the provider is prepaid to cover a patient’s expected healthcare needs over a set timeframe. The capitated payment model ensures a predictable revenue stream for providers while controlling costs for insurers.
Key Characteristics of Capitation:
- Fixed Payments: Providers receive a set fee, usually monthly, for each patient enrolled in a capitated health plan.
- Risk Sharing: The provider takes on financial risk if patient care costs exceed the capitation rate.
- Focus on Prevention: By decoupling payment from service volume, providers are incentivized to keep patients healthier and reduce costly hospitalizations.
- Capitated Claims Meaning: Unlike fee-for-service claims, capitated claims often involve simplified submissions since payments are pre-arranged, reducing administrative overhead.
For example:
- A provider has 1,000 patients enrolled under a capitation contract.
- The capitation rate is $30 PMPM.
- Regardless of whether a patient visits once or 10 times in a month, the provider receives $30 for each patient, totaling $30,000 per month.
This creates financial stability for providers but also places responsibility on them to manage care efficiently, avoid unnecessary services, and invest in preventive strategies.
Types of Capitation in Medical Billing
Capitation isn’t a one-size-fits-all model. Healthcare organizations and payers can structure agreements differently depending on the scope of services covered, the providers involved, and the level of financial risk shared. Below are the main types of capitation in medical billing:
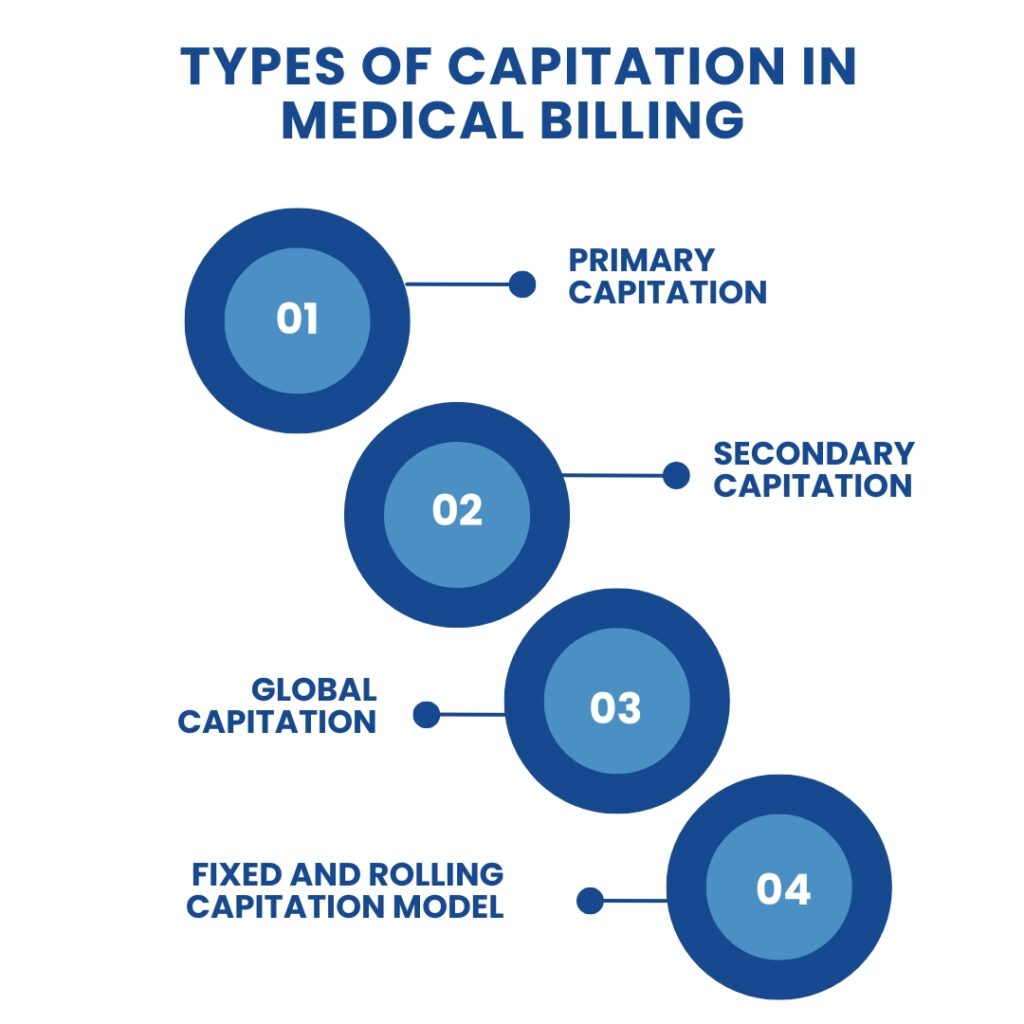
Primary Capitation
In a primary capitation agreement, health insurers pay providers directly for delivering services to enrolled members. This arrangement is common in primary care practices, where the provider receives a per-member, per-month (PMPM) payment to cover preventive, diagnostic, and basic treatment services.
Example: A primary care doctor is paid a fixed monthly fee for each patient under their care, covering routine checkups, immunizations, and lab tests.
Secondary Capitation
In secondary capitation, payments are made to specialists, laboratories, or diagnostic centers out of the funds the primary care provider receives. This ensures that specialized services are also managed under a capitation arrangement rather than billed separately on a fee-for-service basis.
Example: A primary care provider might pay a dermatology clinic a capitated amount to cover all skin-related services for patients under their care.
Global Capitation
Global capitation goes a step further by covering all healthcare services for a defined patient population, including primary care, specialty care, and hospital services. This model places the highest financial risk on providers but also offers the most opportunities for efficiency and care coordination.
Example: An accountable care organization (ACO) accepts global capitation to manage the full spectrum of care for 50,000 patients.
Fixed and Rolling Capitation Model
Another distinction lies in how payments are structured over time:
- Fixed Capitation Model: Providers receive a flat, predetermined payment at regular intervals (usually monthly). This amount remains unchanged regardless of changes in patient volume or service utilization.
- Rolling Capitation Model: Payments are periodically adjusted based on updated enrollment data, risk scores, or service usage patterns. This allows for more flexibility and fairness but adds administrative complexity.
Global Payment vs Capitation
Although the terms are often used interchangeably, global payment and capitation are distinct reimbursement models. Both aim to control healthcare costs and promote accountability, but they differ in structure and scope.
What is Global Payment?
Global payment is a method where providers receive a lump sum payment to cover all the care a patient or a group of patients may need during a specified time period (e.g., a year). This single payment covers hospital services, physician visits, and even post-acute care.
Global Payment vs Capitation: Key Differences
| Aspect | Global Payment | Capitation |
| Scope | Covers all services for a patient population or episode of care. | Covers specific services (e.g., primary care, specialty care, or all services under global capitation). |
| Payment Frequency | Typically, annual or per episode (large lump sum). | Typically, monthly per-member-per-month (PMPM) payments. |
| Risk Distribution | Providers assume responsibility for the total healthcare costs of the defined population. | Providers assume risk only for the services defined in the capitation contract. |
| Flexibility | Broader, covers comprehensive needs across care settings. | It can be narrower, depending on whether the agreement is primary, secondary, or global. |
| Example Use Case | Large health systems or ACOs manage all care for a region. | Primary care practices manage routine and preventive services. |
Capitated Health Plan
A capitated health plan is an insurance arrangement where the payer (usually an HMO, IPA, or ACO) pays providers a fixed, per-member-per-month (PMPM) amount to deliver covered healthcare services to enrolled patients. Instead of paying for each service separately, the insurer shifts financial responsibility to the provider.
This model creates predictable costs for insurers and stable revenue for providers, while encouraging efficient care delivery.
How Capitated Health Plans Work
- Enrollment: Patients sign up for a health plan, and their assigned providers receive capitation payments.
- Payment: Providers are prepaid monthly, regardless of how often patients use services.
- Service Coverage: Contracts outline what services are included (e.g., preventive, diagnostic, or specialty care).
- Risk Pool: Often, a percentage of payments is withheld in a “risk pool,” released at year-end if the provider keeps costs within budget.
Example: Capitation Rate Schedule
Capitation rates are usually age- and risk-adjusted. For example:
| Member’s Age | Capitation per Member, per Month | Withhold (10%) | Final Payment |
| 0–1 | $25.00 | $2.50 | $22.50 |
| 2–4 | $10.00 | $1.00 | $9.00 |
| 5–20 | $5.00 | $0.50 | $4.50 |
| >20 | $15.00 | $1.50 | $13.50 |
This is just an illustrative model, but it shows how payments vary based on demographics and utilization expectations.
Impact on Providers
- Pros: Predictable revenue, simplified billing, and an incentive to focus on preventive care.
- Cons: Higher financial risk if patient needs exceed payments; potential pressure to limit referrals or specialist care.
In short, a capitated health plan transfers financial accountability from the insurer to the provider while aiming to improve efficiency and outcomes.
Capitation vs Other Payment Models
Healthcare reimbursement models come in many forms, each with unique incentives and risks. To understand capitation fully, it’s important to see how it compares with other major payment systems.
Capitation vs Fee-for-Service
Fee-for-service (FFS) is the traditional payment model in which providers are reimbursed for each test, visit, or procedure they perform. In contrast, capitation pays providers a set fee per patient regardless of service volume.
| Aspect | Capitation | Fee-for-Service |
| Payment Basis | Fixed per-member-per-month (PMPM). | Payment for each service or procedure. |
| Incentives | Focuses on prevention, efficiency, and cost control. | Incentivizes more procedures and higher volume. |
| Revenue Predictability | Predictable monthly income. | Income fluctuates with patient visits and procedures. |
| Risk Distribution | Financial risk is on the provider. | Financial risk is on the payer/insurer. |
| Patient Experience | More focus on preventive care; risk of shorter visits. | More services are offered, but potential for unnecessary procedures. |
Fee-for-Service vs Capitation: Pros and Cons
- Pros of Capitation: Predictable revenue, promotes prevention, and reduces unnecessary services.
- Cons of Capitation: Risk of underutilization, pressure on providers to cut costs, and higher risk for small practices.
- Pros of Fee-for-Service: Easier for small practices, providers are fully paid for services delivered, and there is no financial risk if patients need intensive care.
- Cons of Fee-for-Service: Encourages overtreatment, less focus on prevention, unpredictable costs for payers.
Capitation vs Bundled Payment
Bundled payment (also called episode-based payment) reimburses providers a single payment for all services related to a treatment episode (e.g., surgery + recovery). Capitation, on the other hand, covers a broader time-based scope (monthly/annually) across all patient care needs.
| Aspect | Capitation | Bundled Payment |
| Payment Unit | Per patient, per month (PMPM). | Per episode of care (e.g., joint replacement, maternity care). |
| Scope | Continuous care across services and time periods. | Limited to one treatment episode or condition. |
| Risk | Providers bear risk for overall population health. | Providers bear risk for managing costs within an episode. |
| Best Fit | Preventive and chronic care management. | Acute, procedure-based care (surgeries, maternity). |
Benefits of Capitation Model
The capitated payment model has been adopted by many healthcare organizations because it aligns financial incentives with better patient outcomes. Instead of rewarding volume (as in fee-for-service), capitation encourages providers to deliver efficient, preventive, and patient-centered care.
Here are the key benefits of the capitation model:
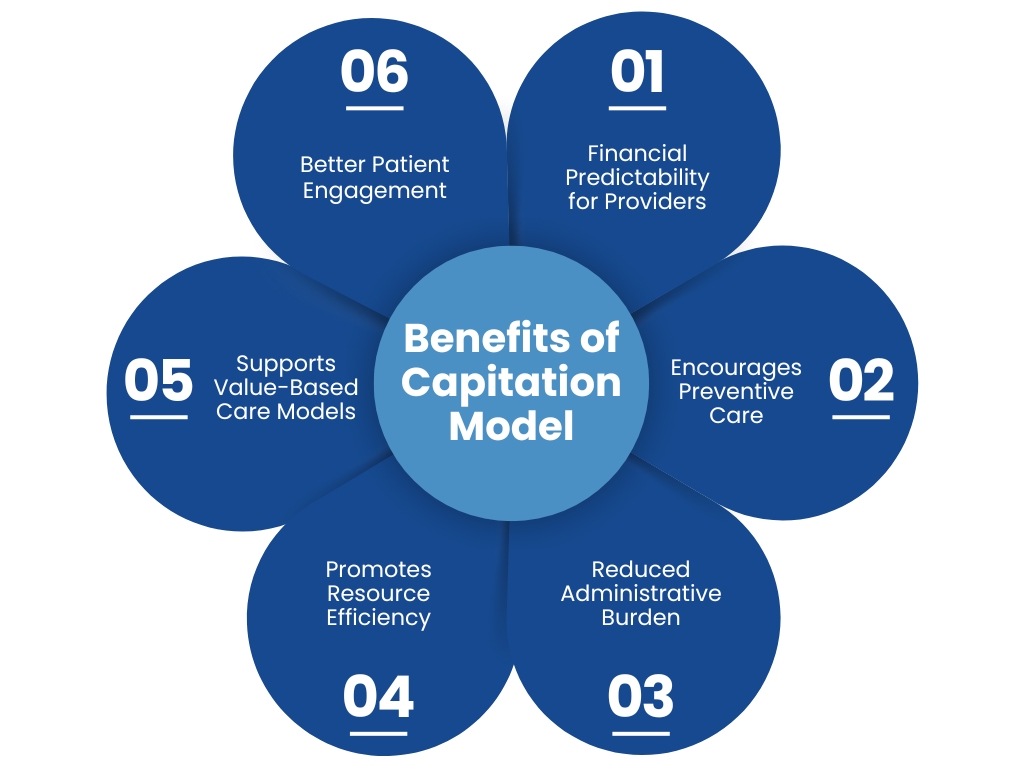
Financial Predictability for Providers
- Providers receive steady, predictable revenue through per-member-per-month (PMPM) payments.
- This financial stability allows practices to budget effectively, hire care managers, and invest in infrastructure.
- Unlike fee-for-service, providers are not penalized during low patient visit periods (e.g., during the COVID-19 pandemic).
Encourages Preventive Care
- Capitation incentivizes providers to keep patients healthy to reduce costly interventions later.
- More focus on wellness visits, vaccinations, screenings, and lifestyle management programs.
- Preventive strategies improve patient outcomes and reduce long-term costs.
Reduced Administrative Burden
- Fewer claims to file since payments are prepaid.
- Less time and money spent on billing disputes, approvals, and reimbursement tracking.
- Providers can focus more on patient care instead of paperwork.
Promotes Resource Efficiency
- Providers are motivated to use diagnostic tests, procedures, and medications judiciously.
- Encourages use of care coordination, telehealth, and multidisciplinary teams.
- Reduces redundancy in testing and duplicate procedures.
Supports Value-Based Care Models
- Capitation shifts the focus from volume to quality of care and outcomes.
- Providers are rewarded for keeping populations healthy rather than simply treating illness.
- Aligns with modern healthcare goals: improved patient experience, reduced costs, and better population health.
Better Patient Engagement
- Since providers are not pressured to bill per service, they can focus on holistic care.
- Capitation allows room for care coordination, patient education, and addressing social determinants of health (housing, food access, mental health support).
Risks and Disadvantages of Capitation in Healthcare
While the capitated payment model offers many benefits, it also comes with challenges that providers and patients need to understand. The model transfers financial risk to providers, which can create unintended consequences if not managed carefully.
Here are the main risks of capitation in healthcare and its disadvantages:
Financial Risk for Providers
- If patient care costs exceed the fixed capitation payment, providers absorb the loss.
- Smaller practices or solo providers may struggle since they lack the patient volume to balance high-cost patients with low-cost ones.
- Unexpected surges in demand (e.g., a flu outbreak) can strain finances.
Risk of Underutilization
- Providers may feel pressured to limit services to keep costs down.
- Patients might receive shorter visits, fewer referrals, or less costly medications.
- While preventive care is encouraged, some patients may experience reduced access to necessary specialist services.
Overutilization of Patients (Quantity over Quality)
- To maximize revenue, providers may enroll as many patients as possible under capitation contracts.
- This can result in longer wait times, shorter visits, and lower-quality interactions.
Risk Selection (Cherry-Picking Patients)
- Providers may avoid enrolling high-cost or complex patients (e.g., those with chronic illnesses).
- This leads to unfair exclusion of patients who need more intensive care, undermining equitable access.
Patient Dissatisfaction
- Patients may perceive capitation as cost-driven rather than patient-driven.
- If they feel rushed during appointments or denied referrals, trust in providers can erode.
Disadvantages of Capitation in Healthcare (Summary)
- For Providers: High financial risk, pressure to control costs, and administrative complexity in managing referrals and contracts.
- For Patients: Potential underutilization of care, reduced access to specialists, and shorter consultations.
- For Healthcare Systems: Requires strong quality monitoring to prevent under-treatment and ensure ethical care delivery.
How Capitated Payments Are Calculated
Capitation rates are not arbitrary; they are carefully structured to balance fairness for providers and cost control for payers. Understanding how capitated payments are determined helps providers prepare for negotiations and financial planning.
Here are the key steps in calculating capitation payments:
Risk Assessment
- Patients differ in their expected healthcare costs.
- Payers assess risk scores based on age, chronic conditions, demographics, and historical healthcare use.
- Example: A patient with diabetes and hypertension has a higher risk score than a healthy 25-year-old, leading to a higher capitation rate.
Historical Data Analysis
- Utilization patterns such as hospital admissions, ER visits, and lab use are reviewed.
- This data helps predict how much care similar patient groups will likely need in the future.
Risk Adjustment
- Risk adjustment ensures fairness by compensating providers more for high-cost patients.
- CMS often uses the Hierarchical Condition Category (HCC) model to standardize adjustments.
Service Coverage Agreement
Contracts define what’s included in the capitation payment:
- Preventive care (screenings, vaccinations).
- Routine visits and diagnostics.
- Sometimes specialty or hospital care (in global capitation).
Services not covered are billed separately under fee-for-service arrangements.
Geographic and Regional Variations
- Capitation rates vary by region due to differences in cost of living, resource availability, and patient demographics.
- Urban providers may receive lower per-patient rates than rural providers because of higher patient volumes.
Negotiation Between Payers and Providers
- Final rates are usually negotiated based on projected needs and historical performance.
- Larger organizations often secure better terms due to economies of scale.
Risk Pool Withhold
Insurers may withhold a percentage of payments (e.g., 10%) into a risk pool.
At the end of the year:
- If providers keep costs below expectations, the withheld funds are released as a bonus.
- If costs exceed expectations, the funds cover the deficit.
Example Calculation (PMPM)
- Provider has 2,000 patients enrolled.
- Capitation rate: $40 per member, per month (PMPM).
- Monthly revenue = 2,000 × $40 = $80,000.
- If 10% is withheld for the risk pool → $8,000.
- Provider receives $72,000/month upfront, with the possibility of reclaiming $8,000 if costs are managed effectively.
Capitation in Practice
Capitation may sound theoretical, but it’s widely used in U.S. healthcare today. Many managed care organizations, health maintenance organizations (HMOs), independent practice associations (IPAs), and accountable care organizations (ACOs) rely on capitation contracts to balance cost control with patient care.
Here’s how capitation works in practice:
Health Maintenance Organizations (HMOs)
- HMOs frequently use primary capitation with contracted physicians.
- Patients must select a primary care provider (PCP) who receives a fixed monthly payment for their care.
- PCPs act as “gatekeepers,” managing referrals to specialists and ensuring cost-effective use of services.
Independent Practice Associations (IPAs)
- IPAs are networks of independent physicians that contract collectively with payers.
- They often negotiate capitated health plan agreements to gain better terms than solo practices could achieve.
- Payments may cover not only primary care but also referrals, labs, and specialist services.
Accountable Care Organizations (ACOs)
- ACOs often experiment with global capitation or hybrid models.
- They manage care for large patient populations, assuming responsibility for both costs and outcomes.
- Capitation gives them the financial flexibility to invest in preventive programs, care coordinators, and telehealth.
Pre-Payment During COVID-19
- When fee-for-service practices struggled due to fewer patient visits, capitated providers had stable revenue.
- This stability allowed them to keep their doors open, hire care managers, and continue preventive care even during a crisis.
Example: Primary Care Practice Under Capitation
- A family practice receives $30 PMPM for 1,500 patients.
- Monthly revenue = $45,000, regardless of visit volume.
The provider uses funds to:
- Hire a nurse care manager.
- Offer patient education sessions.
- Increase preventive screenings.
By reducing unnecessary ER visits and hospitalizations, the practice saves money and improves outcomes.
What Services Are Usually Included?
Most capitation contracts cover:
- Preventive, diagnostic, and treatment services.
- Immunizations and office-administered medications.
- Basic lab tests.
- Health education and counseling.
- Routine vision and hearing screenings.
Some agreements also include:
- Specialty referrals.
- Diagnostic imaging.
- Hospital care (in global capitation models).
Summary
Capitation in medical billing is more than just a payment method; it’s a shift in how healthcare is delivered and financed. By paying providers a fixed, upfront amount per patient, capitation encourages efficiency, prevention, and long-term health management.
Compared to fee-for-service and bundled payments, capitation aligns more closely with the goals of value-based care: improving patient outcomes while controlling costs.
However, capitation also introduces challenges, particularly financial risk for providers, the danger of underutilization, and the potential for patient dissatisfaction if care feels rushed or limited. For smaller practices, these risks may outweigh the benefits without proper support.
The future of healthcare likely lies in hybrid models that blend capitation with other approaches, alongside quality incentives and data-driven care management. For providers who prepare strategically, capitation can deliver predictable revenue, healthier patients, and a stronger role in shaping modern healthcare delivery.