Medical billing can feel like navigating a maze, especially when dealing with specific place of service codes. If you’ve ever wondered about POS 71 in medical billing or struggled with claim denials related to public health clinic services, you’re in the right place.
POS 71 is more than just another billing code—it’s a critical identifier that determines how payers process and reimburse claims for services provided at state or local public health clinics. Whether you’re a seasoned billing professional or new to healthcare revenue cycle management, understanding how to correctly apply and bill this code can make the difference between smooth reimbursements and frustrating denials.
What is POS 71 in Medical Billing?
POS 71 is a place of service code designated specifically for state or local public health clinics. In medical billing, place of service codes are two-digit identifiers that tell insurance payers exactly where a healthcare service was performed. These codes are essential components of claim forms, particularly the CMS-1500 form used for professional billing.
The Centers for Medicare & Medicaid Services (CMS) maintains an official list of place of service codes, and POS 71 holds a unique position as it applies exclusively to government-operated public health facilities at the state or local level.
POS 71 Description and Definition
According to CMS guidelines, the POS 71 description defines it as: “A facility maintained by either state or local health departments that provides ambulatory primary care services, regardless of whether the facility operates on a scheduled or walk-in basis.”
This definition encompasses several key characteristics:
- Government ownership: The facility must be operated by state or local government health departments
- Ambulatory services: Services are provided on an outpatient basis
- Primary care focus: The clinic offers fundamental healthcare services
- Flexible scheduling: Services can be appointment-based or walk-in
Think of POS 71 as the billing code that identifies services delivered in your local county health department clinic or state-run community health centers where residents receive vaccinations, screenings, and primary care services funded by public health programs.
When to Use POS 71 Code
Understanding when to apply POS 71 is crucial for billing accuracy. Use this code when:
- Services are rendered at a state-operated public health clinic
- Treatment occurs at a county or municipal health department facility
- The facility is government-funded and operated (not private or federally qualified)
- Services include preventive care, immunizations, health screenings, or primary care
- The location meets CMS criteria for state or local public health clinics
It’s important to note that POS 71 should not be used for federally qualified health centers (FQHC), which have their own designated place of service codes.
Understanding Place of Service Codes in Medical Billing
Before diving deeper into POS 71, let’s establish why place of service codes matter so much in the medical billing ecosystem.
The Importance of Accurate POS Codes
Place of service codes serve multiple critical functions in healthcare billing:
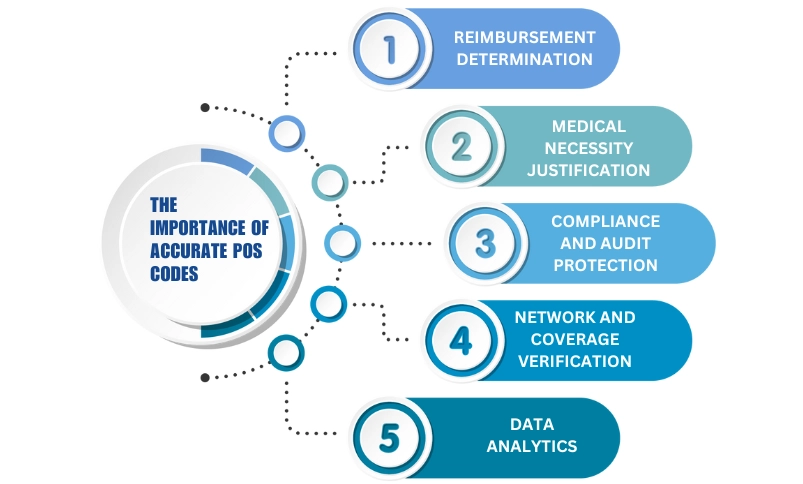
1. Reimbursement Determination: Different locations often have different reimbursement rates. A procedure performed in a hospital outpatient department may reimburse at a different rate than the same procedure in a physician’s office.
2. Medical Necessity Justification: Some services are only covered when performed in specific settings. Using the wrong POS code can trigger automatic denials.
3. Compliance and Audit Protection: Accurate coding demonstrates compliance with billing regulations and protects providers during audits.
4. Network and Coverage Verification: Insurance companies use POS codes to determine if services were provided at in-network or out-of-network facilities.
5. Data Analytics: Healthcare systems and payers use POS codes to track utilization patterns and healthcare delivery trends.
Using an incorrect place of service code isn’t just a minor error—it can result in claim denials, delayed payments, compliance issues, and even allegations of fraudulent billing in severe cases.
Where POS 71 Fits in the Healthcare Setting
In the broader landscape of place of service codes, POS 71 occupies a specific niche. The CMS maintains over 40 different POS codes, each representing distinct healthcare settings:
- POS 11: Office
- POS 20: Urgent Care Facility
- POS 21: Inpatient Hospital
- POS 22: On-Campus Outpatient Hospital
- POS 23: Emergency Room – Hospital
- POS 24: Ambulatory Surgical Center
- POS 31: Skilled Nursing Facility
- POS 49: Independent Clinic
- POS 50: Federally Qualified Health Center
- POS 71: State or Local Public Health Clinic
- POS 72: Rural Health Clinic
POS 71 specifically identifies government-operated public health facilities that serve community health needs, often providing services to underserved populations, offering preventive care programs, and conducting public health initiatives like vaccination campaigns and disease surveillance.
How to Bill POS 71 in Medical Billing
Now that you understand what POS 71 represents, let’s explore the practical steps for billing POS 71 accurately and efficiently.
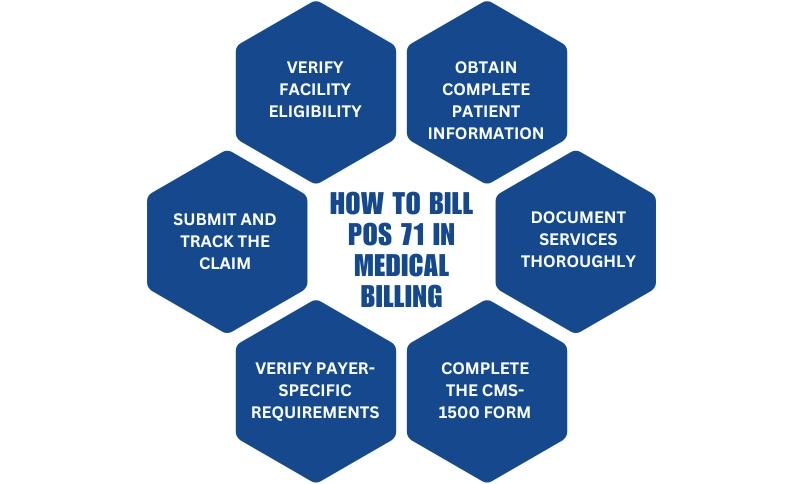
Step-by-Step Guide to Billing POS 71
Step 1: Verify Facility Eligibility
Before using POS 71, confirm that the facility meets all criteria:
- Is it operated by a state or local government health department?
- Does it provide ambulatory primary care services?
- Is it distinct from federal programs like FQHCs?
Step 2: Obtain Complete Patient Information
Gather all necessary patient demographics and insurance information:
- Patient’s full legal name and date of birth
- Current address and contact information
- Insurance policy numbers and group numbers
- Primary and secondary insurance details
- Any applicable public health program enrollment information
Step 3: Document Services Thoroughly
Ensure clinical documentation supports the services billed:
- Detailed provider notes describing the service
- Medical necessity justification
- Specific diagnosis codes (ICD-10)
- Procedure codes (CPT/HCPCS)
- Time and date of service
Step 4: Complete the CMS-1500 Form
When completing the claim form:
- Enter “71” in Box 24B (Place of Service) for each line item
- Include appropriate CPT codes for services rendered
- Link diagnosis codes correctly to justify medical necessity
- Include provider NPI and facility information
Step 5: Verify Payer-Specific Requirements
Different insurance carriers may have unique requirements for POS 71 claims:
- Check if the payer recognizes POS 71 (most do, but verification prevents surprises)
- Review any special documentation requirements
- Confirm prior authorization needs for specific services
Step 6: Submit and Track the Claim
- Submit electronically when possible (faster processing, fewer errors)
- Track claim status regularly
- Follow up on any pending claims within 2-3 weeks
Required Documentation for POS 71 Claims
Proper documentation is the foundation of successful POS 71 billing. Essential documentation includes:
Clinical Documentation:
- Complete SOAP notes (Subjective, Objective, Assessment, Plan)
- Chief complaint and history of present illness
- Examination findings and clinical decision-making
- Treatment plans and patient instructions
Administrative Documentation:
- Patient registration forms with accurate demographic information
- Insurance verification records
- Consent forms for treatment
- Assignment of benefits forms
Billing Documentation:
- Charge tickets or encounter forms
- Service date verification
- Provider credentials and signature
- Facility information confirming it’s a state or local public health clinic
Supporting Documentation (as needed):
- Laboratory reports
- Immunization records
- Screening results
- Referral documentation
Common Payers That Accept POS 71
Most major insurance payers recognize and accept POS 71 for appropriate services:
Government Payers:
- Medicare: Accepts POS 71 for covered services at public health clinics
- Medicaid: State Medicaid programs commonly reimburse POS 71 claims, though requirements vary by state
- State Children’s Health Insurance Program (CHIP)
Commercial Payers:
- Blue Cross Blue Shield plans
- UnitedHealthcare
- Aetna
- Cigna
- Humana
Important Consideration: While most payers accept POS 71, reimbursement rates and coverage policies vary. Always verify benefits before providing services, especially for non-emergent care.
POS 71 vs POS 31: Key Differences Explained
One common source of confusion in medical billing is distinguishing between similar place of service codes. Let’s examine POS 71 vs POS 31 to clarify when each should be used.
What is POS 31?
POS 31 designates a Skilled Nursing Facility (SNF)—a facility that provides skilled nursing care and related services for patients who require medical or nursing care, or rehabilitation services for the rehabilitation of injured, disabled, or sick persons.
POS 31 is used for:
- Long-term care facilities providing skilled nursing
- Rehabilitation services in a skilled nursing environment
- Post-acute care following hospitalization
- Facilities where patients typically reside for extended periods
When to Use POS 71 vs POS 31
The distinction between POS 71 vs POS 31 comes down to facility type and service nature:
| Aspect | POS 71 | POS 31 |
| Facility Type | State or local public health clinic | Skilled nursing facility |
| Ownership | Government-operated | Can be private or government-owned |
| Service Type | Ambulatory/outpatient primary care | Skilled nursing and rehabilitation |
| Patient Status | Walk-in or scheduled outpatient visits | Residents requiring skilled care |
| Typical Services | Vaccinations, screenings, preventive care | Daily nursing care, physical therapy, wound care |
| Duration | Single visit or short-term | Extended stays (weeks to months) |
Billing Scenarios: Choosing the Right Code
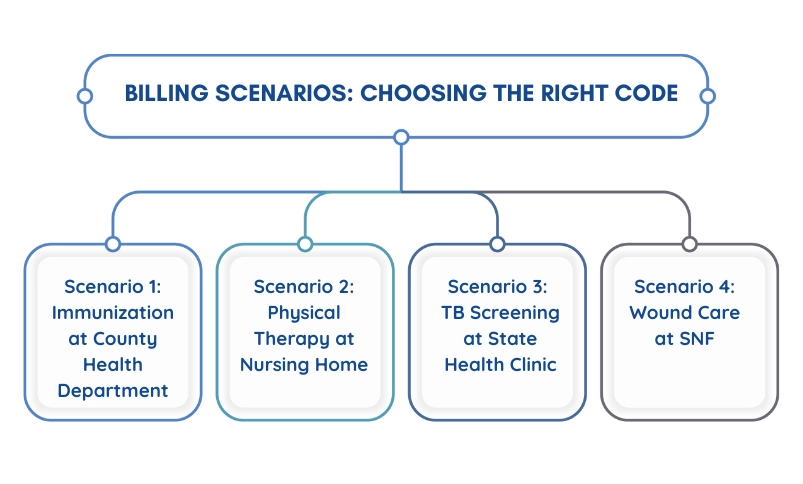
Scenario 1:
Immunization at County Health Department A patient visits the county health department for a flu vaccination.
- Correct Code: POS 71
- Reasoning: Service provided at a local government public health clinic on an outpatient basis
Scenario 2:
Physical Therapy at Nursing Home A patient residing in a skilled nursing facility receives physical therapy.
- Correct Code: POS 31
- Reasoning: Service provided at a skilled nursing facility for a resident
Scenario 3:
TB Screening at State Health Clinic A patient receives tuberculosis screening at a state-operated health clinic.
- Correct Code: POS 71
- Reasoning: Preventive screening at a state public health facility
Scenario 4:
Wound Care at SNF A resident of a skilled nursing facility receives wound care management.
- Correct Code: POS 31
- Reasoning: Skilled nursing service for a facility resident
The key distinction: POS 71 is for outpatient services at government public health clinics, while POS 31 is for services provided to residents of skilled nursing facilities.
Common Services Billed Under POS 71
Understanding which services are typically associated with POS 71 helps ensure appropriate code application and supports medical necessity documentation.
Immunizations and Vaccinations
Public health clinics are primary providers of community immunization services. Common vaccinations billed under POS 71 include:
Routine Childhood Vaccines:
- MMR (Measles, Mumps, Rubella)
- DTaP (Diphtheria, Tetanus, Pertussis)
- Polio vaccine
- Hepatitis A and B vaccines
- Varicella (Chickenpox) vaccine
Adult Immunizations:
- Influenza (flu) vaccines
- Pneumococcal vaccines
- Tdap boosters
- Shingles vaccine
- HPV vaccine
Travel Vaccines:
- Yellow fever
- Typhoid
- Japanese encephalitis
- Meningococcal vaccines
When billing immunizations under POS 71, remember to include both the vaccine product code (from the CPT vaccine codes) and the administration code (90460-90474 series for vaccines).
Preventive Care Services
State and local public health clinics often provide comprehensive preventive services:
Well-Child Visits:
- Developmental screenings
- Growth monitoring
- Health education and counseling
- Early and Periodic Screening, Diagnostic and Treatment (EPSDT) services
Women’s Health Services:
- Family planning counseling
- Contraceptive services
- Pregnancy testing
- STI screening and education
- Breast and cervical cancer screenings
Adult Preventive Services:
- Annual wellness visits
- Cardiovascular risk assessments
- Diabetes screening
- Blood pressure monitoring
- Cholesterol screening
Disease Screening Programs
Public health clinics play a vital role in community disease screening initiatives:
Infectious Disease Screening:
- HIV testing and counseling
- Tuberculosis screening (PPD tests)
- Hepatitis C screening
- Sexually transmitted infection testing
Chronic Disease Screening:
- Diabetes screening programs
- Hypertension screening
- Lead poisoning screening (particularly for children)
- Anemia screening
Cancer Screening Programs:
- Colorectal cancer screening
- Breast cancer screening (mammography referrals)
- Cervical cancer screening (Pap smears)
When billing these services under POS 71, ensure that documentation clearly demonstrates the service was provided as part of a public health initiative at a qualifying facility.
POS 71 Billing Requirements and Compliance
Compliance with billing regulations is non-negotiable in healthcare. Let’s examine the requirements specific to POS 71 billing.
CMS Guidelines for POS 71
The Centers for Medicare & Medicaid Services provides clear guidelines for place of service code usage:
Official Definition Adherence: The facility must meet the CMS definition of a state or local public health clinic. Simply calling a facility a “public health clinic” doesn’t make it eligible for POS 71 if it doesn’t meet ownership and operational criteria.
Accurate Representation: Providers must accurately represent where services were performed. Using POS 71 for services not provided at qualifying facilities constitutes fraudulent billing.
Documentation Standards: Clinical documentation must support that services were medically necessary and appropriate for the public health clinic setting.
Claim Form Completion: POS 71 must be correctly entered in Box 24B of the CMS-1500 form or the electronic equivalent in 837P transactions.
Provider Enrollment: Providers billing under POS 71 must be properly enrolled with payers and credentialed to provide services at the public health clinic location.
State-Specific Regulations
While CMS provides federal guidelines, individual states may have additional requirements for POS 71 billing, particularly for Medicaid claims:
Medicaid Variations: Each state Medicaid program may have unique policies regarding:
- Which services are covered at public health clinics
- Prior authorization requirements
- Documentation standards
- Reimbursement rates
- Billing time limits
State Licensure: Ensure the public health clinic maintains all required state licenses and certifications.
Scope of Practice: Some states limit which provider types can bill certain services at public health clinics.
Vaccine Programs: States often have specific programs (like Vaccines for Children) with unique billing rules that intersect with POS 71 usage.
Best Practice: Consult your state’s Medicaid provider manual and establish direct communication with your state’s Medicaid billing department to understand state-specific POS 71 requirements.
Documentation Best Practices
Robust documentation protects against denials and audit findings:
1. Facility Verification Documentation: Maintain records proving the facility qualifies as a state or local public health clinic:
- Government ownership documentation
- Facility licensure
- Department of Health affiliation letters
2. Clinical Documentation Excellence:
- Use clear, legible notes (electronic health records preferred)
- Document chief complaints thoroughly
- Record examination findings completely
- Justify medical necessity for all services
- Include provider signature and credentials
3. Billing Documentation Accuracy:
- Match diagnosis codes to services provided
- Ensure procedure codes accurately reflect work performed
- Verify dates of service
- Confirm POS 71 is appropriate for each service line
4. Patient Documentation:
- Obtain signed consent for treatment
- Document insurance verification efforts
- Record patient communication about benefits and responsibilities
5. Compliance Program Documentation:
- Regular internal audits of POS 71 usage
- Staff training records on proper code application
- Written policies and procedures for POS 71 billing
- Compliance committee meeting minutes
Common Errors When Billing POS 71
Even experienced billers make mistakes. Let’s identify the most frequent errors with POS 71 and how to avoid them.
Top Denial Reasons for POS 71 Claims
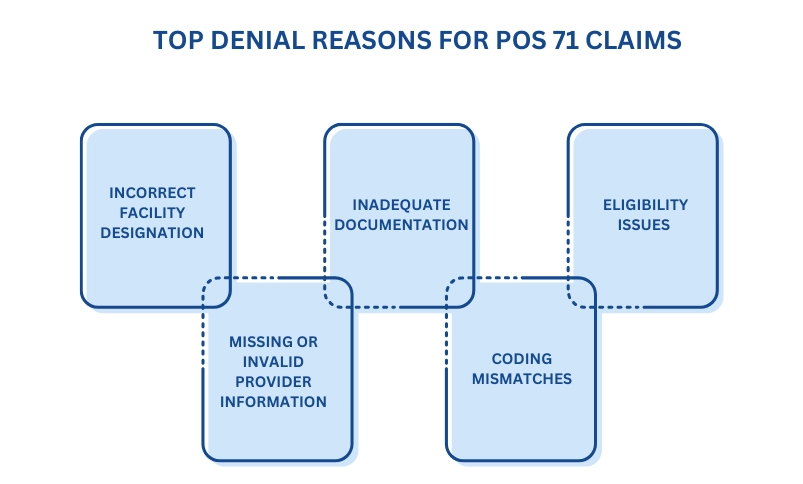
1. Incorrect Facility Designation
The Error: Using POS 71 for facilities that don’t meet CMS criteria, such as:
- Federally Qualified Health Centers (should use POS 50)
- Private clinics (typically POS 11)
- Rural Health Clinics (should use POS 72)
- Hospital-based clinics (POS 22 or 19)
The Impact: Automatic claim denial or incorrect reimbursement rate application.
2. Missing or Invalid Provider Information
The Error:
- Billing provider not enrolled at the public health clinic location
- Missing or incorrect National Provider Identifier (NPI)
- Supervising physician information incomplete
The Impact: Claims rejected for provider eligibility issues.
3. Inadequate Documentation
The Error:
- Missing clinical notes supporting services billed
- No medical necessity justification
- Incomplete patient information
- Missing required signatures
The Impact: Denial for lack of medical necessity or insufficient documentation.
4. Coding Mismatches
The Error:
- Diagnosis codes don’t support procedure codes
- Using outdated or invalid CPT codes
- Bundling errors where separate codes shouldn’t be billed together
- Modifier misuse or omission
The Impact: Denials for coding errors or downcoded payments.
5. Eligibility Issues
The Error:
- Patient not eligible on date of service
- Insurance information incorrect or outdated
- Services not covered for patient’s insurance plan at POS 71
The Impact: Denial for patient eligibility or lack of coverage.
How to Avoid POS 71 Billing Mistakes
Strategy 1: Implement Verification Protocols
Create a pre-service checklist:
- Verify facility meets POS 71 criteria (annual review)
- Confirm patient insurance eligibility before service
- Check provider credentials and enrollment status
- Review coverage for planned services
Strategy 2: Invest in Staff Training
Regular education prevents errors:
- Quarterly training on place of service codes
- Annual compliance reviews
- Updates when CMS guidelines change
- Case study reviews of denied claims
Strategy 3: Use Technology Wisely
Leverage your practice management system:
- Configure default POS 71 for qualifying locations
- Build edit checks that flag potential coding mismatches
- Implement claim scrubbing software before submission
- Use electronic eligibility verification
Strategy 4: Conduct Regular Audits
Internal monitoring catches errors before payers do:
- Monthly chart audits reviewing POS 71 usage
- Quarterly coding accuracy assessments
- Annual comprehensive compliance audits
- Denial pattern analysis
Strategy 5: Establish Clear Communication
Connect all stakeholders:
- Clinical staff understand documentation requirements
- Front desk staff verify eligibility accurately
- Billing team knows when to use POS 71
- Management receives regular compliance reports
Correcting Rejected POS 71 Claims
When a POS 71 claim is denied, swift action is essential:
Step 1: Analyze the Denial Reason
Review the Explanation of Benefits (EOB) or Electronic Remittance Advice (ERA):
- What was the specific denial code?
- Is it a coding error, documentation issue, or eligibility problem?
- Is additional information requested?
Step 2: Gather Supporting Documentation
Collect everything needed to support your appeal:
- Complete medical records
- Proof of facility eligibility for POS 71
- Insurance verification documentation
- Relevant clinical guidelines or policies
Step 3: Correct and Resubmit or Appeal
Choose the appropriate path:
For Correctable Errors: If the denial resulted from a fixable mistake (wrong code, missing modifier), correct and resubmit as a corrected claim.
For Valid Claims Incorrectly Denied: File a formal appeal with:
- Cover letter explaining why the claim should be paid
- Supporting documentation
- Reference to payer policies supporting your position
- Timeline of service and submission
Step 4: Track and Follow Up
Monitor your corrected claim or appeal:
- Set calendar reminders for follow-up (typically 30 days)
- Document all communication with payers
- Escalate to provider representatives if needed
- Consider peer-to-peer review for complex denials
Step 5: Learn and Prevent
Use denials as learning opportunities:
- Update internal procedures to prevent similar errors
- Share findings with relevant staff
- Modify documentation templates if needed
- Adjust coding practices based on payer feedback
POS 71 Reimbursement Rates and Considerations
Understanding the financial implications of POS 71 helps practices manage revenue expectations and make informed business decisions.
How POS Codes Affect Reimbursement
Place of service codes significantly impact reimbursement in several ways:
Facility vs. Non-Facility Rates: Medicare and many commercial payers use different fee schedules based on practice expense. Services billed at facilities with lower overhead (like physician offices) typically reimburse at higher rates than services at facilities with higher overhead (like hospital outpatient departments).
POS 71 Positioning: State or local public health clinics generally receive reimbursement rates similar to office settings (POS 11) or slightly adjusted based on payer policies. However, this varies by payer and service type.
Rate Determination Factors:
- Type of service provided
- Payer contracts and negotiated rates
- Geographic location (through geographic practice cost indices)
- Provider type (physician vs. non-physician practitioner)
Medicare Reimbursement for POS 71: Medicare generally applies the non-facility rate to services at public health clinics, though this can vary by service. The Medicare Physician Fee Schedule (MPFS) determines specific reimbursement amounts.
Medicaid Reimbursement for POS 71: State Medicaid programs have considerable flexibility in setting rates for public health clinic services. Many states provide enhanced reimbursement for preventive services and immunizations delivered at public health facilities to encourage community health initiatives.
Insurance Coverage for POS 71 Services
Coverage for services at state or local public health clinics varies by payer and service type:
Preventive Services: Most payers, including Medicare and Medicaid, provide robust coverage for preventive services at POS 71 facilities:
- Immunizations (often at 100% coverage with no cost-sharing)
- Screening services (covered under preventive care mandates)
- Well visits and health assessments
Primary Care Services: Basic primary care visits at public health clinics are typically covered, though:
- Prior authorization may be required for some services
- Coverage limits may apply (visit frequency restrictions)
- Cost-sharing (copays, deductibles) varies by plan
Specialized Services: Coverage for specialized services depends on:
- Whether the service is within the typical scope of public health clinics
- Payer network agreements
- Medical necessity documentation
Coverage Verification: Always verify benefits before providing services, as:
- Commercial plans may have network restrictions
- Some services may require referrals or prior authorization
- Patient cost-sharing varies significantly by plan
Reimbursement Strategy for POS 71 Providers:
- Understand Your Payer Mix: Know which payers you serve most frequently and their specific POS 71 policies.
- Negotiate Thoughtfully: When contracting with commercial payers, ensure POS 71 reimbursement rates are clearly defined and fair.
- Maximize Preventive Service Revenue: Take full advantage of well-covered preventive services to maintain healthy revenue streams.
- Document Medical Necessity: Robust documentation justifies higher-level services and protects against downcoding.
- Monitor Reimbursement Patterns: Regularly review actual payments vs. expected payments to identify discrepancies or opportunities.
Conclusion
Successfully navigating POS 71 in medical billing requires a combination of knowledge, attention to detail, and commitment to compliance. As we’ve explored throughout this comprehensive guide, POS 71 serves a specific and important purpose in healthcare billing—accurately identifying services provided at state or local public health clinics.
If you’re looking to strengthen your POS 24 billing accuracy and maintain full compliance, RevenueES can help. Our experienced billing specialists ensure every outpatient surgery claim is properly coded, fully documented, and reimbursed at its true value. Connect with us today to enhance your billing performance and protect your revenue cycle.