Behind every successful healthcare practice lies one silent hero, “credentialing.” It’s the process that proves your providers are who they say they are: qualified, licensed, and ready to deliver care patients can trust. But in the world of medical billing, credentialing isn’t just about trust; it’s about getting paid.
Without proper credentialing, claims get denied, reimbursements stall, and even the most skilled physicians find themselves tangled in red tape. On the other hand, a well-structured credentialing process ensures compliance, strengthens your reputation, and keeps your revenue cycle flowing seamlessly.
What Is Medical Credentialing?
Medical credentialing is the formal process of verifying that healthcare providers, doctors, nurses, therapists, or any medical professionals have the proper qualifications, training, and licenses to deliver care.
In essence, it’s a quality assurance mechanism that ensures patients are treated by competent, accredited professionals.
For healthcare organizations and payers, credentialing serves as proof that a provider meets the standards required to offer safe, ethical, and effective care. Without it, providers can’t legally bill insurance companies, participate in payer networks, or even work within hospitals.
Credentialing vs. Privileging vs. Enrollment
These three terms are often confused but serve different functions:
| Process | Purpose | Outcome |
| Credentialing | Verification of education, training, and licenses | Confirms qualifications |
| Privileging | Grants authority to perform specific procedures | Defines the scope of practice |
| Enrollment | Registers providers with insurance networks | Enables billing and payment |
Example:
A surgeon must first be credentialed to prove their medical qualifications, then privileged to perform surgeries, and finally enrolled with payers like Medicare or private insurers to receive reimbursements.
Why Credentialing in Medical Billing Is So Important
Credentialing goes beyond compliance; it’s the backbone of your entire revenue cycle. Here’s why it matters so much:
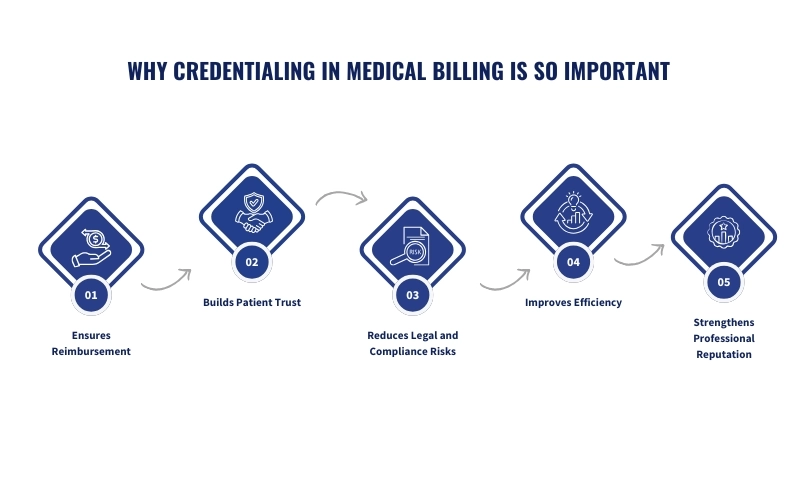
Ensures Reimbursement
Insurance companies require verified credentials before approving claims. If a provider isn’t credentialed, claims can be denied or delayed, causing significant revenue loss.
Builds Patient Trust
Patients feel safer when they know their healthcare provider’s qualifications are verified and up to date. Credentialing reinforces that trust and strengthens your practice’s reputation.
Reduces Legal and Compliance Risks
Credentialing ensures that every provider meets state and federal requirements, reducing exposure to malpractice claims, audits, or penalties for non-compliance.
Improves Efficiency
With verified providers, billing and claims processing become faster and smoother. This reduces administrative burdens and supports a healthy revenue cycle management (RCM) process.
Strengthens Professional Reputation
Being a credentialed provider gives a sense of legitimacy in the eyes of peers, payers, and patients alike. It reflects professionalism and commitment to quality care.
Types of Credentialing in Medical Billing
Credentialing isn’t one-size-fits-all. There are several types designed to fit different scenarios and practice setups.
1. Initial Credentialing
This is the first step for any new healthcare provider joining a facility or payer network. It involves verifying education, licenses, work experience, malpractice history, and certifications before granting permission to treat patients or submit claims.
2. Recredentialing
Credentialing doesn’t last forever. Providers must go through recredentialing every 2–3 years to ensure ongoing compliance with industry standards. This periodic re-verification ensures that licenses remain active and no disciplinary actions have been taken against the provider.
3. Individual Credentialing
Individual credentialing is done for solo practitioners who wish to bill payers under their own National Provider Identifier (NPI) and Tax ID. It offers flexibility and independence but requires more hands-on management.
4. Group Credentialing
Group credentialing allows multiple providers within a single organization or practice to apply together under one Tax ID. It simplifies paperwork and ensures that if one provider leaves, the group’s credentialing status remains intact.
The Complete Credentialing Process in Medical Billing
Understanding the step-by-step credentialing process helps you prevent errors, avoid delays, and maintain compliance with payer requirements.
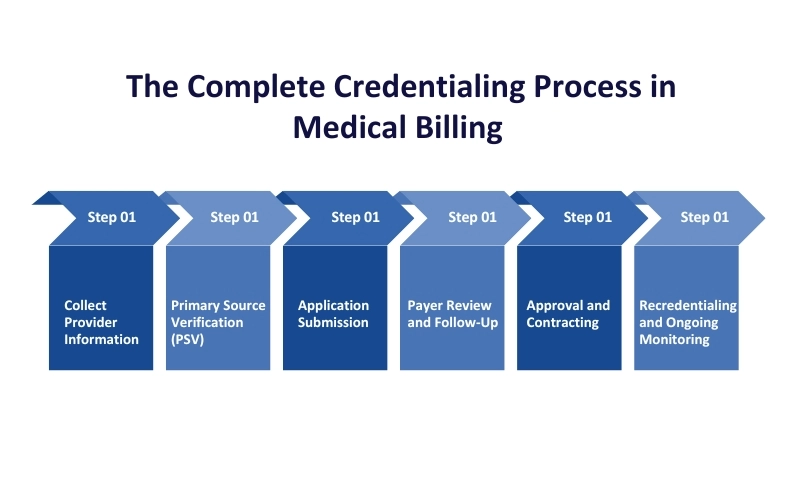
Step 1: Collect Provider Information
The process starts with gathering detailed provider information and supporting documents, including:
- Medical school diplomas and residency certificates
- Active medical licenses
- Board certifications
- Work history and professional references
- Malpractice insurance details
- DEA certificate and NPI number
- Updated CV or resume
Most payers and networks require a CAQH (Council for Affordable Quality Healthcare) profile. Keeping it updated saves time and avoids resubmissions.
Step 2: Primary Source Verification (PSV)
Verification from the primary source ensures that the credentials are genuine. This involves contacting:
- Medical schools and training programs
- State medical boards
- Previous employers and hospitals
- Licensing authorities
- Federal exclusion lists, such as OIG and SAM
These checks protect patients, prevent fraud, and uphold healthcare integrity.
Step 3: Application Submission
After collecting and verifying documents, the next step is submitting the credentialing application to insurance payers. Depending on the payer, this can be done:
- Electronically (via portals like CAQH or payer websites)
- Or via paper applications
It’s crucial to double-check for accuracy; a single typo or missing document can delay approval by weeks.
Step 4: Payer Review and Follow-Up
Once submitted, payers review the application and may request additional details or clarifications.
Regular follow-ups are vital during this stage. Staying proactive helps you identify issues early and keeps your application from being lost in the queue.
Step 5: Approval and Contracting
After successful verification, the provider is approved and granted network participation. The next step involves contract negotiation, reviewing payment terms, fee schedules, and agreement conditions.
Once both parties sign, the provider can officially start seeing patients and billing insurance.
Step 6: Recredentialing and Ongoing Monitoring
Credentialing isn’t a one-time task. Providers must maintain compliance by updating credentials regularly, renewing licenses, and re-attesting CAQH information.
Automating reminders or using credentialing software can prevent costly lapses in status.
Insurance Credentialing: The Backbone of Reimbursement
What Is Insurance Credentialing?
Insurance credentialing is the process that allows healthcare providers to become part of an insurer’s network. It ensures that the provider meets the insurer’s standards for education, training, and professional conduct.
Without insurance credentialing, providers cannot bill or receive payment from insurance companies, even if the patient has coverage.
Common Steps in Insurance Credentialing
- Identify the Insurance Providers: Make a list of payers you want to join (Medicare, Medicaid, Blue Cross, Aetna, etc.).
- Prepare Documentation: Each payer requires specific forms, such as tax information, malpractice details, and licenses.
- Complete CAQH Registration: Major payers use CAQH for credentialing. Providers must complete their profiles and re-attest quarterly.
- Submit the Application: Double-check every section for accuracy before submission.
- Follow-Up and Clarify Queries: Communication with payer representatives is essential to avoid unnecessary delays.
Credentialing Timelines and Common Delays
Typically, credentialing takes 60 to 120 days, but delays can happen due to:
- Missing or incorrect documents
- Incomplete CAQH profiles
- Lack of communication with payers
- Errors in provider data
Staying proactive with follow-ups and maintaining updated documentation can help reduce these bottlenecks.
Key Elements of a Credentialing Checklist
A well-prepared credentialing checklist ensures that nothing gets missed during the verification process. Missing even a single document can delay approvals for weeks, so organization is key.
Here’s what a comprehensive credentialing checklist should include:
- Personal Information (Full name, SSN, address, and contact details)
- National Provider Identifier (NPI) and Tax ID Number
- Medical License Copies (active and in good standing)
- DEA and Controlled Substance Certificates
- Board Certification(s)
- Education and Training Certificates (medical school, internship, residency, fellowship)
- Work and Practice History (with start and end dates)
- Malpractice Insurance and Claims History (10 years)
- Professional and Personal References
- Hospital Privileges and Affiliations
- Medicare and Medicaid Numbers
- CAQH Profile and Attestation
- OIG and SAM Exclusion Check Reports
- Immunization and Health Records (if required)
Common Mistakes to Avoid During Credentialing (Infographic)
Credentialing is often a long, detail-heavy process, and even small mistakes can cause big financial consequences. Below are some of the most common errors that delay or derail approvals:
Data Entry Errors: Simple typos in NPI numbers, incorrect dates of employment, or mismatched license details can result in application rejection. Always double-check every entry before submission.
Missing Information: Leaving any section blank or forgetting to attach supporting documents (like malpractice insurance or license copies) is one of the top causes of delays.
Poor Documentation Management: Disorganized record-keeping makes it difficult to locate documents during payer audits or recredentialing periods.
Ignoring Recredentialing Deadlines: Most payers require recredentialing every 2–3 years. Missing deadlines can lead to the deactivation of provider status and temporary revenue loss.
Lack of Follow-Up: Submitting the application isn’t enough. Regularly checking in with payers ensures the process doesn’t get stuck in limbo.
Compliance Oversight: Credentialing requirements differ by state and payer. Failing to meet these unique standards can result in compliance issues or denials.
Role of Medical Billing Companies in Credentialing
Credentialing can consume hundreds of administrative hours per year, especially for growing practices. That’s why many healthcare organizations outsource credentialing to professional medical billing and credentialing companies like RevenueES.
Benefits of Outsourcing Credentialing
- Time Savings: Experts handle paperwork, verifications, and follow-ups.
- Error Reduction: Credentialing specialists are familiar with payer requirements, minimizing rejections.
- Faster Approvals: Dedicated teams ensure timely communication with insurance networks.
- Compliance Assurance: They stay updated with regulatory changes and renewals.
- Revenue Stability: Providers can focus on care delivery while billing and credentialing are handled efficiently.
How Outsourced Credentialing Works
- The provider submits all necessary documents.
- The credentialing team verifies, completes, and submits applications to payers.
- Regular follow-ups and progress updates are maintained.
- Once approved, the billing team integrates the credentials into the payer network for claims submission.
Outsourcing doesn’t just save time, it directly improves cash flow by accelerating payer enrollment and minimizing claim denials.
Credentialing and Compliance Regulations
Credentialing isn’t just an administrative formality; it’s a compliance requirement governed by federal and state-level standards. Understanding these regulations helps avoid penalties and maintain payer trust.
Key Regulatory Bodies
- NCQA (National Committee for Quality Assurance): Sets credentialing standards for healthcare organizations.
- CMS (Centers for Medicare & Medicaid Services): Regulates federal program participation.
- OIG (Office of Inspector General): Monitors exclusions and fraud risks.
- SAM (System for Award Management): Ensures providers aren’t involved in disqualifying activities.
- HIPAA (Health Insurance Portability and Accountability Act): Protects patient data during credentialing and billing.
Common Compliance Requirements
- Verify all credentials via Primary Source Verification (PSV).
- Maintain updated CAQH and payer data.
- Conduct background checks for malpractice or disciplinary actions.
- Store credentialing records securely to comply with HIPAA.
Remaining compliant not only keeps your practice audit-ready but also strengthens payer relationships and patient trust.
Final Thoughts
Credentialing in medical billing is more than just paperwork; it’s the heartbeat of your revenue cycle. When done right, it keeps your practice compliant, your reimbursements on time, and your reputation strong.
From collecting provider data to maintaining CAQH attestation and following up with payers, each step requires precision and persistence. But with a streamlined process, or the help of expert credentialing services, you can eliminate delays, avoid costly denials, and ensure your practice continues to grow confidently.
Need help managing your credentialing process?
Partner with a trusted medical billing and credentialing team for credentialing services to save time, stay compliant, and get paid faster, so you can focus on what matters most: your patients.