Efficient, compliant billing is the backbone of every successful healthcare organization, and one regulation that stands at its core is the 72 Hour Rule in Medical Billing. Often misunderstood, this rule can significantly affect hospital reimbursements, compliance audits, and claim accuracy.
Whether you’re a billing manager, compliance officer, or healthcare provider, understanding how the Medicare 72-hour rule works can protect your facility from costly errors and compliance risks.
In this article, we’ll break down the rule in plain language, explain its exceptions, show real-world examples, and share practical tips to help you stay fully compliant with CMS guidelines for inpatient admission while ensuring every dollar you’ve earned is properly reimbursed.
What is the 72 Hour Rule in Medical Billing?
The 72 Hour Rule in Medical Billing, often referred to as the Medicare 72-Hour Rule or 3-Day Payment Window Rule, is a regulation established by the Centers for Medicare & Medicaid Services (CMS).
Under this rule, any outpatient diagnostic or related services performed within 72 hours before a patient’s hospital admission must be bundled into the inpatient claim, rather than being billed separately.
In simpler terms, if a patient receives certain tests or procedures within three days before being admitted to the same hospital, those services are considered part of the inpatient stay, not separate outpatient visits.
Key Purpose of the Rule
The main goal of this regulation is to:
- Prevent double-billing and overpayments to hospitals.
- Ensure Medicare pays accurate reimbursements for bundled services.
- Maintain billing transparency across hospital systems.
This rule primarily applies to hospitals and entities that are wholly owned or wholly operated by the admitting hospital.
Example:
A patient visits the outpatient department for a CT scan on Monday and is admitted to the same hospital for surgery on Wednesday.
The CT scan must be included (bundled) in the inpatient claim under the Medicare 72-hour rule rather than being billed separately.
Purpose and Importance of the Medicare 72 Hour Rule
The Medicare 72 Hour Rule was created to streamline billing accuracy and reduce fraud under the False Claims Act. By requiring hospitals to combine outpatient and inpatient claims when appropriate, CMS ensures that healthcare providers do not unintentionally (or intentionally) receive duplicate payments.
Why It Matters for Hospitals
- It protects hospitals from compliance violations and potential audits.
- It reduces administrative burden by clarifying when to bundle claims.
- It enhances trust between healthcare providers and payers like Medicare.
The impact of the 72-hour rule on hospital billing compliance is substantial. Failing to adhere can result in overpayment recovery, fines, or claim rejections. That’s why proper education and billing system checks are critical for compliance teams.
CMS Guidelines for Inpatient Admission and the 3-Day Payment Window
According to CMS guidelines for inpatient admission, hospitals must determine whether outpatient services provided before admission are related or unrelated to the inpatient stay.
If the outpatient services are diagnostic or clinically related, they must be included in the inpatient bill. If the services are non-diagnostic and unrelated, they can be billed separately under Medicare Part B.
The 3-Day (72-Hour) Payment Window Includes:
- The date of inpatient admission, and
- The three calendar days immediately prior to that date.
This rule ensures that all services related to the patient’s condition leading to admission are captured under a single, complete inpatient claim.
Diagnostic vs. Non-Diagnostic Services: What’s Included and Excluded
One of the most confusing parts of the 72 Hour Rule in Medical Billing is differentiating between diagnostic and non-diagnostic services. This distinction determines whether a service should be bundled or billed separately.
1. Diagnostic Services (Bundled under the Inpatient Claim)
Diagnostic services are tests or procedures used to identify the cause of a patient’s symptoms or condition. If provided within 72 hours before admission, they must be bundled into the inpatient claim.
Common Diagnostic Services Include:
- Laboratory tests
- Radiology and imaging (X-ray, MRI, ultrasound, etc.)
- Nuclear medicine
- CT scans
- Cardiology studies (EKG, EEG)
- Anesthesia
- Osteopathic manipulative services
2. Non-Diagnostic Services (May Be Billed Separately)
Non-diagnostic or therapeutic services can be billed separately if they are unrelated to the inpatient admission.
Examples Include:
- Physical or occupational therapy
- Counseling sessions
- Routine wellness visits
- Preventive screenings
Example Scenario:
If a patient attends a physical therapy session two days before being admitted for an unrelated cardiac surgery, the therapy is not related to the hospital admission and can be billed separately.
Understanding this diagnostic vs non-diagnostic in 3-day payment window distinction is crucial for accurate and compliant billing.
What Are the Three Exceptions to the Medicare 72-Hour Rule?
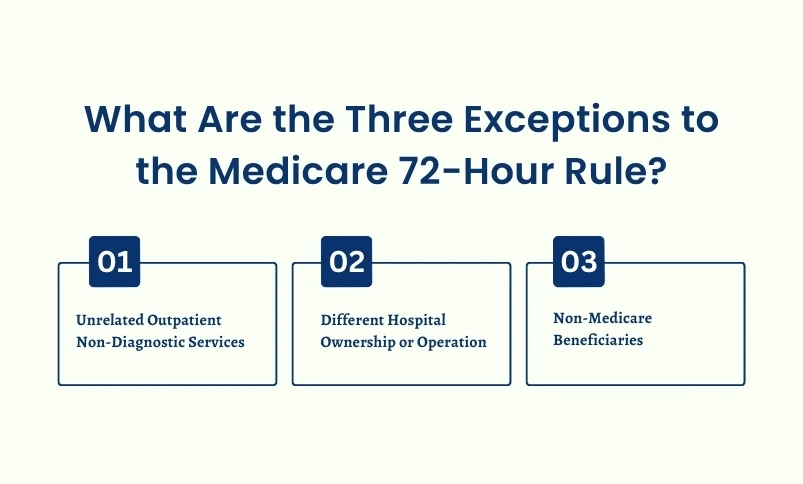
While the rule is broad, there are specific exceptions where outpatient services do not have to be bundled with inpatient claims.
Unrelated Outpatient Non-Diagnostic Services: If the outpatient services are unrelated to the inpatient admission (for example, a dermatology visit before an orthopedic surgery), they can be billed separately under Medicare Part B.
Different Hospital Ownership or Operation: The Medicare 72 hour rule applies only to services provided by entities wholly owned or operated by the admitting hospital. If the outpatient service was provided by a clinic that is not affiliated, the rule does not apply.
Non-Medicare Beneficiaries: The 72-hour rule applies specifically to Medicare patients. Commercial insurers or Medicaid programs may have their own versions, but the federal Medicare rule is distinct.
Does the 72 Hour Rule Apply to Medicaid or Other Payers?
This is a common question among billing professionals: Does the 72-hour rule apply to Medicaid?
The answer is not universally. While Medicare enforces the 72-hour bundling rule nationwide, Medicaid programs are state-administered and may choose to adopt, modify, or ignore this rule based on their own reimbursement structures.
In some states, Medicaid has a similar “payment window” policy, but in others, claims are processed independently. Therefore, always verify through your state Medicaid guidelines or Medicaid Administrative Contractor (MAC) before applying the same logic used for Medicare claims.
Medicare 72 Hour Rule Examples (Real-World Scenarios)
Understanding the rule becomes much easier when you see it applied in practical cases. Here are some clear examples that illustrate when to bundle and when to bill separately.
Example 1: Diagnostic Service – Bundled
A patient visits the outpatient lab for blood work on Monday and is admitted for gallbladder surgery on Wednesday.
✅ The lab work must be included in the inpatient claim (bundled).
Example 2: Non-Diagnostic Service – Unbundled
A patient receives a physical therapy session two days before being admitted for a scheduled cardiac procedure.
✅ The physical therapy is unrelated to the inpatient stay and may be billed separately.
Example 3: Different Facility – Not Bundled
A patient has an X-ray done at an independent imaging center (not owned by the admitting hospital) within 72 hours of admission.
✅ Since the facility is not owned or operated by the hospital, the 72-hour rule does not apply.
These Medicare 72 hour rule examples highlight how important it is for hospitals to correctly identify ownership relationships and service relevance when preparing claims.
Compliance Challenges and Common Mistakes
While the Medicare 72 Hour Rule seems straightforward, many hospitals struggle with its application in real-world billing processes. Misunderstanding or misclassifying services can lead to overpayments, underpayments, and compliance penalties.
Common Billing Mistakes Include:
- Failing to bundle diagnostic outpatient services that are related to an inpatient admission.
- Incorrectly identifying non-diagnostic services as diagnostic, leading to overbundling.
- Overlapping claim submission dates that confuse payers and delay reimbursement.
- Inadequate documentation to prove the relatedness or unrelatedness of outpatient services.
These errors can trigger CMS audits or Office of Inspector General (OIG) investigations. To avoid financial loss and compliance breaches, hospitals must ensure robust internal billing audits, regular staff education, and proper EHR system configuration to flag related outpatient encounters automatically.
Days Claims Payable and Timeliness
Noncompliance with the 72 Hour Rule can also impact days’ claims payable (DCP), a key performance indicator in revenue cycle management.
Incorrect bundling or claim rejections extend claim resolution times, directly affecting cash flow and operational efficiency.
Tools and Techniques to Ensure 72-Hour Rule Compliance
As healthcare billing grows more complex, hospitals are turning to technology-driven solutions to improve compliance with the Medicare 72 Hour Rule.
Best Practices for Compliance:
- Implement EHR Alerts: Configure your electronic health record system to flag any outpatient encounter within three days of an inpatient admission.
- Use Computer-Assisted Audit Techniques (CAATs): These tools scan for separate claims that should have been bundled, helping identify potential compliance risks.
- Staff Training and Education: Regularly train coding and billing teams on CMS guidelines for inpatient admission and 3-day payment window protocols.
- Create a Written Policy: Establish a documented internal policy outlining how preadmission services are reviewed, coded, and billed.
Benefits of Automation
Automated compliance tools not only help prevent errors but also reduce the administrative burden on billing staff. They ensure that claims are bundled correctly, which minimizes rework, appeals, and potential penalties.
How to Stay Updated with CMS 72 Hour Rule Guidelines
The Centers for Medicare & Medicaid Services (CMS) frequently updates its billing and compliance policies to reflect changes in law, technology, and fraud prevention strategies. Staying current is essential for compliance officers and billing professionals.
Recommended Steps to Stay Updated:
- Review CMS Publications: Regularly check official CMS documents like MLN Matters® SE20024, which provides in-depth clarification of the 72-hour rule.
- Subscribe to CMS Newsletters: Sign up for Medicare Learning Network (MLN) updates and CMS email alerts.
- Join Professional Billing Associations: Organizations like HFMA and AAPC provide timely updates, webinars, and certification programs.
- Conduct Annual Policy Reviews: Reassess internal billing procedures annually to ensure they align with the latest CMS rules.
By maintaining proactive awareness, hospitals can ensure continued compliance and avoid unnecessary claim denials or penalties.
Why the 72 Hour Rule Matters for Hospital Financial Health
Beyond compliance, the 72 Hour Rule directly impacts a hospital’s financial performance and operational efficiency.
Key Impacts Include:
- Prevention of Overbilling: Ensures that Medicare is not charged twice for related services.
- Optimized Revenue Integrity: Proper bundling leads to faster reimbursements and fewer rework cycles.
- Audit Readiness: Accurate billing documentation helps hospitals pass CMS audits with confidence.
- Operational Clarity: Consistent billing processes reduce confusion across departments.
By fully understanding and implementing the Medicare 72 Hour Rule, healthcare organizations can maintain trust with payers, safeguard their financial stability, and enhance compliance culture throughout the organization.
Record Keeping and Documentation Standards
Accurate documentation is the foundation of compliance with the Medicare 72-Hour Rule. Each inpatient claim must include complete details to verify the inclusion (or exclusion) of outpatient services within the 3-day payment window.
Essential Documentation Elements:
- Primary diagnosis and any comorbid conditions
- Procedures performed during inpatient stay
- Dates and times of all outpatient and inpatient encounters
- Patient demographics (age, gender, admission/discharge details)
- Evidence linking outpatient services to inpatient admission reasons
Proper record keeping allows hospitals to justify their billing decisions during audits and maintain transparency with payers.
Summing Up
The 72 Hour Rule in Medical Billing is far more than a technicality; it’s a cornerstone of Medicare compliance and ethical billing practice. By understanding how to properly bundle diagnostic services, apply the right exceptions, and follow CMS guidelines, hospitals can reduce risk, streamline billing, and ensure every claim stands up to scrutiny.
Compliance with this rule not only prevents over payments and audit flags but also enhances operational efficiency and financial health. In a rapidly evolving healthcare landscape, mastering the Medicare 72 Hour Rule isn’t optional; it’s essential for sustainable success.
FAQ’s
- Unrelated outpatient non-diagnostic services.
- Services provided by facilities not owned or operated by the admitting hospital.
- Non-Medicare patients (commercial or Medicaid payers).