When it comes to behavioral health billing, every code matters, especially add-on codes like CPT 90833. Used for psychotherapy provided alongside evaluation and management (E/M) services, this code can significantly impact reimbursement if billed correctly. But here’s the catch: missing modifiers, incomplete documentation, or pairing it with the wrong E/M code can lead to denials and lost revenue.
In this guide, we’ll explore what CPT code 90833 is, how to bill it, which codes it pairs with, reimbursement rates, and the most common mistakes practices make, so you can maximize payment and stay fully compliant.
What is CPT Code 90833?
The 90833 CPT code description provided by the American Medical Association defines it as psychotherapy, 16 to 37 minutes when performed with an evaluation and management service.
That means CPT code 90833 is not a stand-alone code. It is an add-on code that must be billed with an eligible E/M service. In other words, you can only use it when psychotherapy is delivered during the same encounter where you are also providing medical evaluation or medication management.
This code falls under Psychotherapy Services and Procedures and is most often used by psychiatrists, psychiatric nurse practitioners, and other behavioral health providers who combine medical management with therapy.
When to Use CPT 90833
You should bill CPT 90833 when:
- You spend 16 to 37 minutes providing psychotherapy during a session that also includes medical evaluation or medication management.
- The psychotherapy service is clearly distinct and documented separately from the medical management portion.
- The therapy is evidence-based or supportive, such as cognitive behavioral therapy, motivational interviewing, or supportive psychotherapy.
CPT code 90833 time frame is key. If the therapy is less than 16 minutes, you should not bill 90833. If it goes longer than 37 minutes, you should consider using 90836 (38–52 minutes) or 90838 (53 minutes or more).
Can 99214 and 90833 Be Billed Together?
This is one of the most common provider questions, and the answer is yes.
99214 represents an established patient E/M visit, while 90833 represents psychotherapy that occurs within the same appointment. When billed together, this combination captures both the medical management and the therapeutic time spent with the patient.
To get reimbursed properly:
- Always attach modifier 25 to the E/M code to show that the medical management service is significant and separately identifiable from the psychotherapy.
- Document the time spent on therapy and the type of therapeutic intervention used.
- Keep medical and psychotherapy notes distinct for audit readiness.
In terms of reimbursement, billing 99214 with 90833 can generate around 200 to 250 dollars per session, depending on your payer contracts and location.
Can 90792 and 90833 Be Billed Together?
The answer here is no.
90792 already includes both the psychiatric diagnostic evaluation and psychotherapy components. Since psychotherapy is built into 90792, adding 90833 would be considered duplicate billing.
If you are performing an initial psychiatric diagnostic evaluation, stick with 90792 only. Use 90833 later for ongoing visits when psychotherapy is provided alongside medication management or other E/M services.
Other E/M Codes and 90833 Billing Rules
Not all E/M codes can be billed with psychotherapy add-on codes. Here is a quick reference:
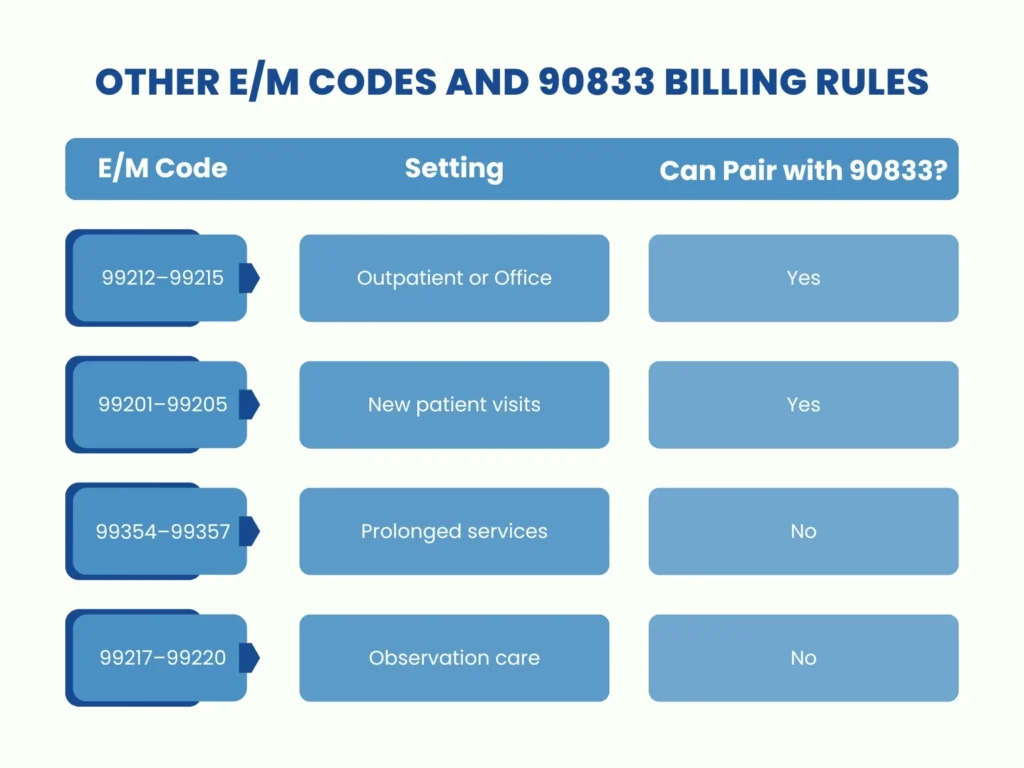
The takeaway is simple. 90833 can only be billed with specific outpatient or new patient E/M codes. It cannot be paired with observation care or prolonged service codes. Always confirm with your payer to avoid denials.
Reimbursement for CPT 90833
Understanding reimbursement for CPT code 90833 is essential to maximizing revenue.
On average, the national reimbursement rate for 90833 ranges from 85 to 110 dollars. When paired with a common E/M service such as 99214, the combined reimbursement can total 200 to 250 dollars per visit.
These figures are estimates. Actual rates vary by:
- Insurance payer (Medicare, Medicaid, commercial plans)
- Geographic location
- Provider type and credentials
- Contracted agreements
For practices that regularly combine psychotherapy with medication management, billing 90833 with E/M codes can significantly improve revenue, provided documentation is accurate and modifiers are applied correctly.
Common Billing Mistakes with CPT Code 90833 (and How to Avoid Them)
Even experienced practices lose money on CPT 90833 due to small but costly errors. Here are the most frequent mistakes and how to fix them:
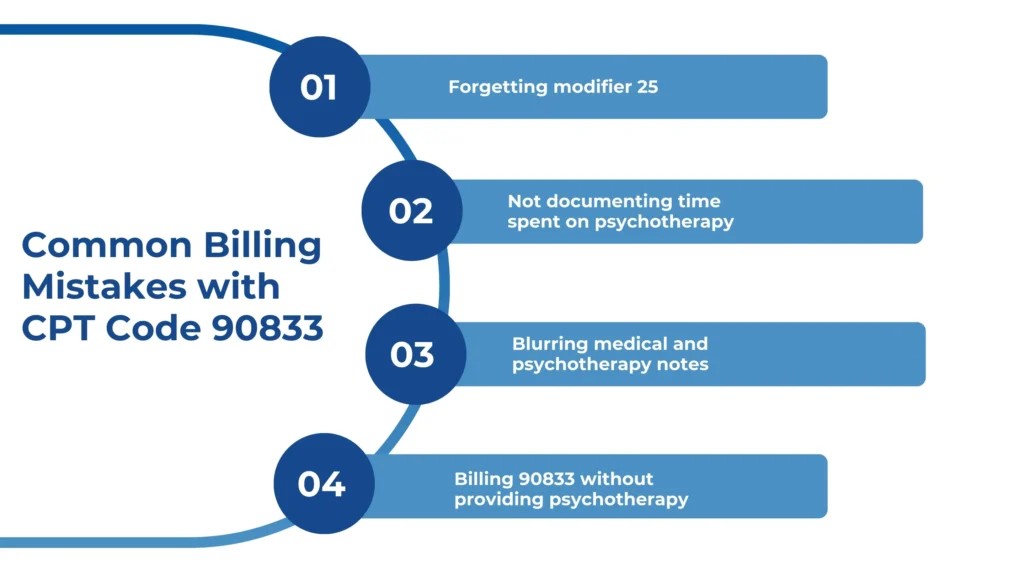
Forgetting modifier 25: Always append modifier 25 to the E/M code when billing with 90833. Without it, insurers may deny the claim.
Not documenting time spent on psychotherapy: Simply stating “psychotherapy provided” is not enough. Document the exact time, such as “25 minutes of cognitive behavioral therapy.”
Blurring medical and psychotherapy notes: Keep medical management notes separate from psychotherapy documentation. This shows a clear distinction between services.
Billing 90833 without providing psychotherapy: You cannot bill this code if only medication management was done. Use it only when psychotherapy is actually provided.
Correcting these errors will not only reduce denials but also protect your practice during audits.
Compliance and Documentation Tips
For 90833 CPT code compliance, clear and thorough documentation is critical. Best practices include:
- Break down the visit by separating the medical management portion from psychotherapy. Example: 15 minutes for med management and 20 minutes of cognitive behavioral therapy.
- Identify the psychotherapy type, such as CBT, supportive therapy, or motivational interviewing.
- Record total time spent specifically on psychotherapy.
- Use structured note templates to make compliance easier and ensure consistent documentation across providers.
This level of detail not only supports reimbursement but also strengthens patient records and audit readiness.
The Bottom Line
Correctly billing the 90833 CPT code can mean the difference between denied claims and steady revenue. If you are unsure whether your practice is fully compliant, or if you want to maximize reimbursement while staying audit-ready, now is the time to act.
👉 Need expert guidance on mental & behavioral health billing? Contact our medical billing specialists today and let us help you streamline claims, reduce denials, and increase revenue.
Key Takeaways
- CPT 90833 is a psychotherapy add-on code for 16 to 37 minutes of therapy provided with an E/M service.
- It must be billed with eligible E/M codes, such as 99214, and always with modifier 25.
- It cannot be billed with 90792, since that code already includes psychotherapy.
- National reimbursement averages 85 to 110 dollars for 90833 alone, and significantly more when paired with E/M.
- Documentation is the most important factor in avoiding denials and maximizing payment.