When you’ve worked hard to provide quality care, the last thing you want is for your payment to be denied because of a missed deadline. Unfortunately, that’s exactly what happens when medical claims aren’t submitted within the timely filing limit. Every payer, from Medicare and Medicaid to BCBS and commercial insurance plans, enforces strict claim-filing deadlines, and even a single day’s delay can turn a reimbursable claim into lost revenue.
The good news? You don’t have to lose sleep over filing timelines anymore. Whether you’re wondering “How long does a provider have to submit a claim to insurance?” or trying to understand the 72-hour rule in medical billing, this complete guide will walk you through everything you need to know.
You’ll learn exactly how to meet every timely filing limit, how to avoid CO-29 denials, and how to build a reliable billing workflow that keeps your reimbursements flowing, fast, clean, and compliant.
What Is a Timely Filing Limit in Insurance Claims?
The timely filing limit is the maximum amount of time a healthcare provider has to submit a claim to an insurance company after delivering services. Think of it as a “claim filing deadline.” If you miss it, the payer can deny the claim regardless of how valid or well-documented the service was.
So, is there a time limit for medical billing?
Absolutely. Each insurance company sets its own timeframe for claim submission, which can range from 30 days to 1 year from the date of service (DOS).
For instance, if a doctor sees a patient on January 10 and their payer allows 90 days to file, the claim must reach the insurer by April 10. If it’s submitted on April 15, it will likely receive a CO-29 denial, meaning the timely filing limit has expired.
Timely filing rules don’t just apply to initial claims. They often extend to corrected claims, appeals, and retroactive billing (for example, when Medicaid eligibility is backdated).
Why Timely Filing Is Critical for Healthcare Providers
Submitting claims on time isn’t just a box to check; it’s one of the most important parts of the medical billing cycle. Missing even one insurance timely filing window can cost hundreds or thousands of dollars in lost reimbursements.
Here’s why it matters so much:
1. Faster Reimbursements
The earlier you file, the faster you get paid. Submitting claims within the time limit for medical billing helps maintain steady cash flow, allowing you to pay staff, vendors, and other operational costs without delay.
2. Higher Claim Acceptance Rates
Payers prioritize clean, timely claims. Submitting within their window significantly reduces the chances of denials.
3. Compliance and Contractual Obligations
Most payer contracts include a timely filing limit clause, typically 90 to 180 days. Missing it means violating that agreement, which can harm your payer relationships.
4. Avoiding Patient Frustration
When claims are denied, patients often receive unexpected bills. Filing on time ensures smoother experiences for both the provider and the patient.
5. Protecting Your Revenue
Filing late means no payment period. Insurance companies rarely grant exceptions, which makes timely claim management essential for keeping your practice profitable.
When Does the Timely Filing Clock Start?
This is one of the most common areas of confusion among billers and providers. The timely filing clock typically starts from the date of service (DOS), but the exact starting point can vary depending on the type of service or payer.
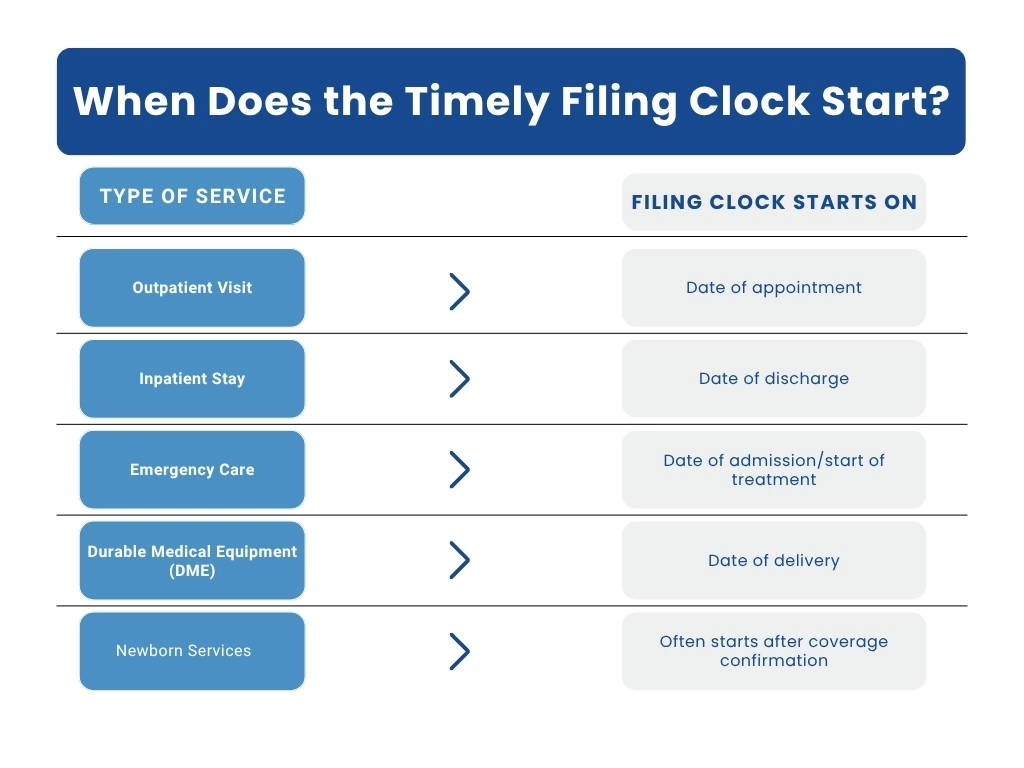
For secondary or tertiary claims, the filing window typically begins on the date of primary payer determination, not the original date of service.
This distinction is vital, especially for providers handling coordination of benefits (COB) or retroactive Medicaid enrollments.
Example: If Medicare pays a claim on March 1 and the secondary payer allows 60 days for submission, your secondary claim must be filed by April 30, not by the date of service.
Common Timely Filing Limits by Major Payers (2025 Update)
Each payer defines its own filing rules. Below is an updated reference list of timely filing limits for major insurance companies in 2025. Always confirm the latest limits directly from provider manuals or payer portals.
Table 1: Major Payers’ Timely Filing Limits
| Insurance Payer | Timely Filing Limit (From Date of Service) | Notes |
| Medicare | 12 months | “How long do you have to bill Medicare?” – 1 year |
| Medicaid | 90–365 days | Varies by state; check your Medicaid timely filing limit |
| UnitedHealthcare | 90–180 days | Commercial and state-specific |
| Cigna | 90–180 days | Out-of-network providers often have extended windows |
| Aetna | 120–180 days | May vary by plan type |
| Kaiser Permanente | 90 days | Verify per region |
| TRICARE / Champus | 1 year | Standard across most plans |
| Humana | 90 days | Commercial and Medicare Advantage |
| Medical Mutual | 1 year | |
| Magellan Health | 60 days | One of the shortest limits |
BCBS Timely Filing Limits by State
Blue Cross Blue Shield (BCBS) plans vary widely depending on the state and plan type, including federal BCBS. The table below outlines the most common BCBS timely filing limits across regions:
| State / Plan | Timely Filing Limit | Notes |
| BCBS Florida (Florida Blue) | 1 year | Applies to most commercial plans |
| BCBS Illinois | 180 days | Consistent across HMO and PPO plans |
| BCBS Texas | 95 days | One of the shortest windows |
| BCBS North Carolina | 18 months | Generous compared to other states |
| BCBS Alabama | 2 years | Longest window among BCBS plans |
| Federal BCBS | 12 months | FEHB program standard |
| BCBS Arizona | 1 year | |
| BCBS Michigan | 180 days (1 year for Complete Plans) | |
| BCBS Massachusetts | 90 days (HMO/PPO), 1 year (Indemnity) | |
| Horizon BCBS New Jersey | 180 days | |
| BCBS New York | 1 year |
Because BCBS operates independently in each state, its timely filing limit rules by payer can differ significantly. Always confirm requirements in your state’s BCBS provider manual.
Example: The federal BCBS timely filing limit under the Federal Employees Health Benefits Program (FEHB) is 12 months, while BCBS Alabama allows a full 2 years, a huge difference if you’re operating across multiple states.
Special Timely Filing Rules: 72-Hour Rule & Out-of-Network Filing
Not all deadlines are created equal. Some payers enforce additional rules that can affect when and how you submit claims.
The 72-Hour Rule in Medical Billing
The 72-hour rule applies primarily to hospital inpatient claims. It requires hospitals to bundle all outpatient services provided within 72 hours prior to an inpatient admission into one claim.
Failing to follow this rule can trigger denials or payment delays, even if the timely filing window hasn’t expired.
Out-of-Network Timely Filing Period
Out-of-network providers often face different, sometimes stricter, timelines. Some plans allow extra time (up to 180 days) to accommodate claim routing, while others shorten the period.
If you’re out of network, make sure to check:
- The exact out-of-network timely filing period is in your payer contract.
- Whether you need to submit via paper or electronically.
- Any special documentation required for reimbursement?
Missing an out-of-network deadline can permanently forfeit your payment rights, even if you provided life-saving care.
Understanding Timely Filing Denials (CO-29 Code Explained)
Even the most experienced billers occasionally face denials, but few are as frustrating as a CO-29 denial.
CO-29 means “The time limit for filing has expired.” In other words, the claim was submitted after the payer’s timely filing limit, so the insurance company won’t pay it, even if every other detail is correct.
Common Reasons for CO-29 Denials:
- Claim not submitted before the claim filing deadline
- Missing or incorrect patient insurance data
- Clearinghouse transmission issues or rejections
- Provider not credentialed at the time of service
- Resubmitting a rejected claim too late
Timely Filing Patient Responsibility
Most payers do not allow providers to bill the patient for claims denied due to missed timely filing. The loss is typically absorbed by the provider. However, exceptions can apply in certain out-of-network timely filing period cases if the patient was informed in advance.
How to Appeal Late or Denied Claims?
If your claim gets denied due to a timely filing limit, all hope isn’t lost. Many payers have appeal or reconsideration processes, as long as you have the documentation to back it up.
Step-by-Step Guide to Appealing a Timely Filing Denial
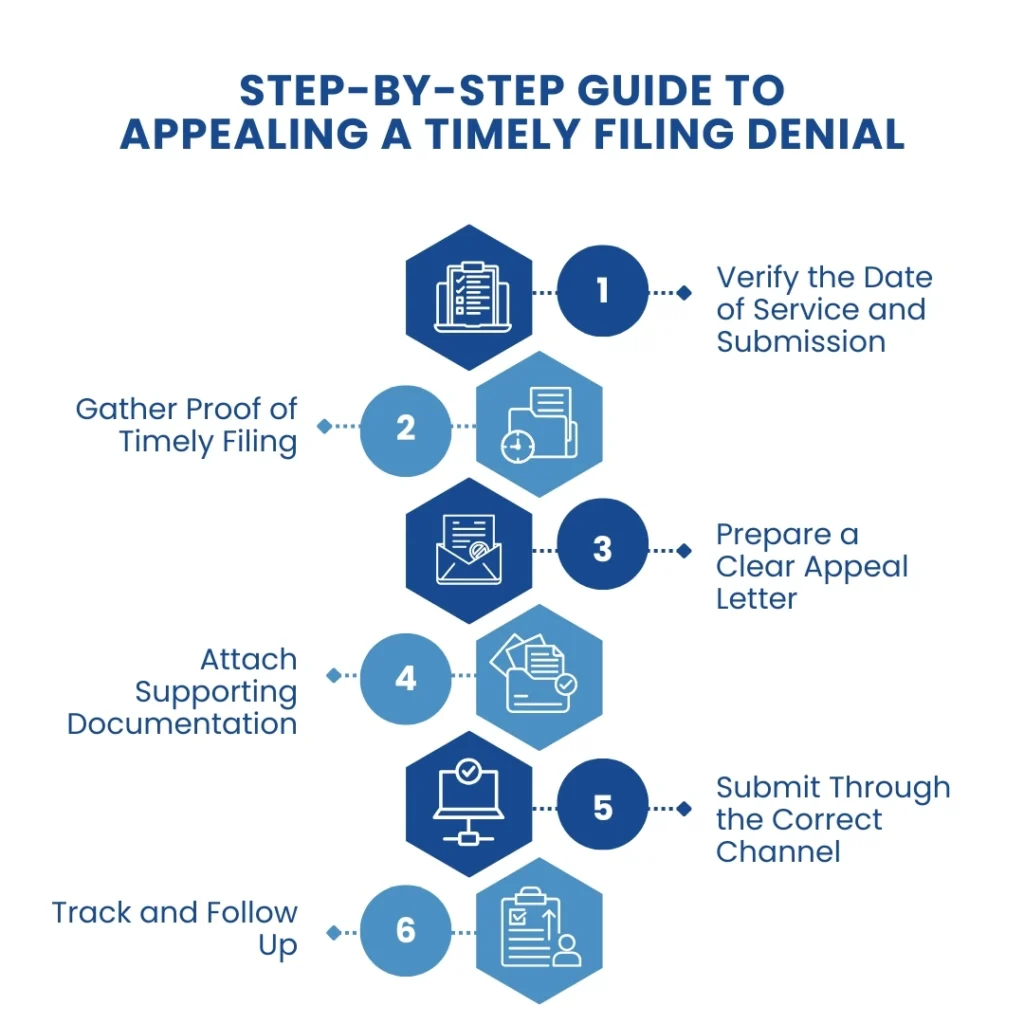
Verify the Date of Service and Submission: Check EHR records or clearinghouse logs to confirm when the claim was transmitted.
Gather Proof of Timely Filing: This might include submission reports, payer acknowledgment receipts, or claim acceptance confirmations.
Prepare a Clear Appeal Letter: Include the reason for late submission, proof of earlier filing, and any relevant communication with the payer.
Attach Supporting Documentation: EOBs, eligibility verification, and reference numbers strengthen your appeal.
Submit Through the Correct Channel: Follow the payer’s official appeal submission method; some require a specific form or fax/email format.
Track and Follow Up: Don’t let appeals vanish in the system. Follow up every 15–30 days until a resolution is received.
Even if you’re past the deadline, still submit the claim. This creates a record and may keep the case eligible for reconsideration, especially for Medicaid retroactive eligibility or payer processing delays.
Common Causes for Missing Timely Filing Deadlines
Knowing what causes missed deadlines can help prevent them altogether. Here are the most frequent culprits behind untimely submissions:
- Incomplete documentation or delayed provider charting
- Missing or inaccurate patient insurance data
- Clearinghouse rejections that go unnoticed
- Lack of prior authorization or incorrect claim routing
- Provider credentialing delays
- Staff unaware of payer-specific limits
- Poor tracking of claim status and denials
Efficient billing teams know exactly how many claims a biller should work per day to stay ahead, typically 25 to 40 claims, depending on payer mix and complexity.
Smart Strategies to Stay Ahead of Filing Deadlines
Timely filing isn’t just about working faster; it’s about working smarter.
Here’s how top-performing billing teams ensure they never miss a filing limit again:
1. Build a Payer Deadline Tracker
Create a spreadsheet or dashboard listing:
- Payer name
- Time limit to submit a health insurance claim
- Claim type (initial, corrected, appeal)
- Submission format (paper or electronic)
- Contact info and escalation pathway
2. Automate and Streamline
Use an EHR or practice management system that alerts you when claims approach their timely filing limit. Automation reduces manual errors and keeps your claims flowing smoothly.
3. Audit Aging Claims Weekly
Review open claims by date of service, not the date entered. Focus on payers with shorter limits like Magellan (60 days) or BCBS Texas (95 days).
4. Train Your Clinical Team
Timely billing starts with timely documentation. Encourage providers to complete and sign notes promptly so the billing cycle starts on time.
5. Monitor Clearinghouse Reports
Rejected claims at the clearinghouse level don’t pause the clock; the timely filing countdown keeps running. Monitor rejections daily and correct them immediately.
6. Understand Timely Filing Limit Rules by Payer
Each payer’s rules differ. For instance:
- Medicaid timely filing limit varies by state (e.g., 95 days in Texas, 12 months in Florida).
- The Federal BCBS timely filing limit is generally one year.
- Medicare allows 12 months from the date of service.
The Bottom Line
Mastering the timely filing limit insurance claim process isn’t just about avoiding denials; it’s about building a smooth, reliable revenue cycle. Every on-time submission means faster reimbursements, fewer write-offs, and more time to focus on patient care instead of paperwork.
FAQ’s
Ans: Each state defines its own.
- Texas Medicaid: 95 days
- Florida Medicaid: 12 months
- California Medicaid: 6 months