Managing a home health agency comes with enough challenges, shrinking margins, staffing gaps, and compliance worries, without the added hit of surprise payment reductions. If you’ve ever wondered why a well-documented, high-quality episode still got reimbursed at a fraction of the expected rate, chances are LUPA is the culprit.
LUPA (Low Utilization Payment Adjustment) is one of the trickiest parts of Medicare’s PDGM payment system. It’s not just about counting visits; it’s about how your patient’s case-mix drives the LUPA threshold and how effectively your team aligns care delivery with those rules.
Miss a visit late in the period, and suddenly your reimbursement shifts from a full episodic rate to per-visit payment.
What Is LUPA? (LUPA medical term)
LUPA (Low Utilization Payment Adjustment) is a payment reduction in Medicare home health when total completed visits in a 30-day payment period fall below the assigned LUPA threshold for that patient.
Medicare expects a certain number of visits (based on patient complexity) during each 30-day period. If you don’t reach that number, the episode is paid per visit instead of the full case-mix episodic amount.
The LUPA medical term is widely used operationally to flag at-risk episodes: “This period is trending toward LUPA, act now.”
Old vs. new rules (why this still trips people up):
- Before 2020 (HH PPS): 60-day episode; a LUPA was 4 or fewer visits, simple, fixed rule.
- Now under PDGM: 30-day periods with variable thresholds (2–6 visits) depending on patient characteristics. That variability is what creates risk and opportunity.
LUPA isn’t about doing “more visits for the sake of it.” It’s about aligning clinically appropriate frequency with the PDGM case-mix expectations so outcomes and reimbursement both stay on track.
How LUPA Works Under PDGM (PDGM visit utilization)
PDGM at a Glance
- Payment is organized into 30-day periods.
- Each period is grouped into a case-mix (HIPPS) that predicts resource use; this is where PDGM visit utilization assumptions live.
- The model front-loads intensity because patients typically benefit from more engagement early after admission.
What Drives the LUPA Threshold?
Each 30-day period’s LUPA threshold is set by the case-mix grouping, which is derived from:
- Admission source & timing: Institutional vs. community; early vs. later periods.
- Clinical grouping: Why the patient needs home health (e.g., wound care, MSK rehab, endocrine).
- Functional impairment (OASIS): Low/medium/high functional need affects expected services.
- Comorbidity adjustments: None/low/high depending on additional diagnoses.
Why PDGM Visit Utilization Matters
- The expected visit pattern under PDGM influences your threshold.
- When clinically appropriate, front-loading in the first 2 weeks can stabilize symptoms, reduce avoidable events, and reduce LUPA risk.
Risk signal: A missed visit in week 3 – 4 (without rapid reschedule) can flip an otherwise compliant period into LUPA.
LUPA Thresholds Explained (+ LUPA threshold calculator)
What Is a LUPA Threshold?
The minimum number of completed visits needed in a 30-day period to receive the full case-mix payment. If you finish below that number, the period becomes a LUPA and pays per visit.
- Typical range: 2 – 6 visits per 30-day period (varies by case-mix).
Mini “Calculator” You Can Use Today
You probably already have this in your EMR, but if you want a quick mental model, follow this 4-step LUPA threshold calculator workflow:
1. Identify the case-mix group
From your EMR: clinical group, admission source & timing, functional score (OASIS), and comorbidity level.
2. Look up the assigned threshold
Your EMR displays it; if not, reference your PDGM tables.
3. Plan frequency to meet/exceed threshold
Schedule threshold + 1 buffer to absorb cancellations.
4. Track daily; reschedule missed visits quickly
A same-week make-up often saves the period.
Rule of thumb: Schedule to meet the lupa threshold by day 21–24 when clinically appropriate. That gives you a safety window before day 30.
Illustrative Examples (not case-rate promises)
- SN-only, low complexity: thresholds often on the lower end (e.g., 3–4).
- Therapy-heavy, moderate complexity: thresholds closer to the higher end (e.g., 5–6).
LUPA & Medicare: Coverage, Rules, and Common Pitfalls
Under LUPA Medicare rules in PDGM, each 30-day period is evaluated separately. If total completed visits are below the threshold, payment converts to per-visit instead of the full episodic amount. Two adjacent 30-day periods for the same patient can have different thresholds based on changing case-mix (e.g., early vs. subsequent period).
Common Ways Agencies Trigger LUPA
- Patient refusals/cancellations (holidays, transportation, caregiving conflicts).
- Scheduling gaps or staffing constraints (therapist availability; weekend coverage).
- Frequency order confusion (vague or outdated orders; missed clarifications).
- OASIS/coding errors (functional scoring or diagnosis sequencing that misplaces the case-mix).
- Late rescheduling (missed visits not rebooked within the 30-day window).
Treat every missed visit as a same-day task for rescheduling. The longer it waits, the higher your LUPA risk.
Real-World LUPA Scenarios & Outliers
Post-Hospital CHF (Moderate Complexity)
- EMR shows a threshold of 5.
- Four visits completed; one last-minute cancellation on day 26 wasn’t rescheduled.
- Result: period drops to per-visit payment, a sizable revenue haircut despite strong clinical work.
SN-Only Weekend Miss
- Low threshold case (e.g., 3 – 4).
- Weekend nurse can’t cover; visit slips past day 30.
- Result: unexpected LUPA on what looked like a “safe” period.
Therapy-Heavy Case, Single Miss
- Threshold 5 – 6 with multiple disciplines.
- One PT visit missed due to availability; reschedule falls into the next period.
- Result: full episodic payment forfeited for the current period.
Pattern to watch: cases with tight discipline availability and patients who prefer specific time windows. Build buffers into the plan of care.
LUPA Billing Requirements (What to Document & Verify)
LUPA billing requirements boil down to proving that your visit frequency, clinical need, and documentation match what was billed, and that you’ve handled exceptions correctly.
Core Documentation Checklist
- Physician orders with clear frequency and any updates signed/timed.
- Accurate, timely OASIS (especially M1800 functional items).
- Diagnosis coding: primary reason for care + comorbidities accurately sequenced.
- Visit documentation: date, duration, discipline, skilled interventions, patient response, progress toward goals.
- Missed visit notifications to the physician when required, with reason and follow-up plan.
Period verification: confirm lupa threshold met before billing; if not, ensure per-visit expectations are coded and supported.
Pre-Bill Sanity Checks
- Reconcile scheduled vs. completed visits and confirm the count.
- Validate the HIPPS/case-mix is correct (no coding/OASIS issues that shift thresholds).
- Confirm any frequency changes are ordered, signed, and reflected in the EMR.
- If LUPA is inevitable, ensure the claim clearly supports per-visit payment and the medical record explains shortfall causes (e.g., repeated patient refusals).
Compliance cue: Even when billing per visit, the medical necessity and skilled need must be obvious from your notes. Thin documentation is a denial magnet.
LUPA Compliance in Home Health Care
Goal: build a repeatable system that prevents avoidable LUPAs, documents unavoidable ones, and withstands audit scrutiny.
Policy & Process (your compliance backbone)
Written LUPA policy: Define monitoring cadence (e.g., daily dashboards + weekly huddles), roles (scheduler, clinical manager, biller), and escalation paths when an episode is two visits or fewer away from the LUPA threshold with <7 days remaining.
Standard operating procedures (SOPs):
- Missed visit SOP: same-day reschedule attempt, physician notification rules, client outreach script, and documentation steps.
- Frequency change SOP: when clinical status shifts, how to obtain updated orders, and who verifies that EMR reflects the new plan.
EMR alerts: automate risk flags (e.g., “Day 20 with two visits remaining”) and require a resolution note before staff can close the day’s tasks.
Training & Governance
- Clinician orientation: teach how PDGM visit utilization influences thresholds, the purpose of front-loading, and when it’s clinically appropriate.
- Scheduler playbooks: templates for building care plans that meet/exceed thresholds with a +1 buffer, plus backup slot rules for high-risk patients.
- Biller & QA alignment: pre-bill checklists; monthly LUPA trend reviews to spot root causes (discipline shortages, holiday dips, order ambiguity).
Technology & Automation
- Electronic content management: auto-generate physician notifications for missed/refused visits, with timestamps and audit trails.
- Dashboards: real-time count of scheduled vs. completed visits, periods nearing day 30, and patients with multiple cancellations.
- Audit-ready exports: one-click packets containing orders, OASIS, visit notes, missed-visit communications, and threshold verification.
Compliance tip: document why a reschedule couldn’t occur (e.g., patient out of town, weather, hospitalization). That context preserves medical necessity and explains shortfalls.
Proven Strategies to Avoid LUPA
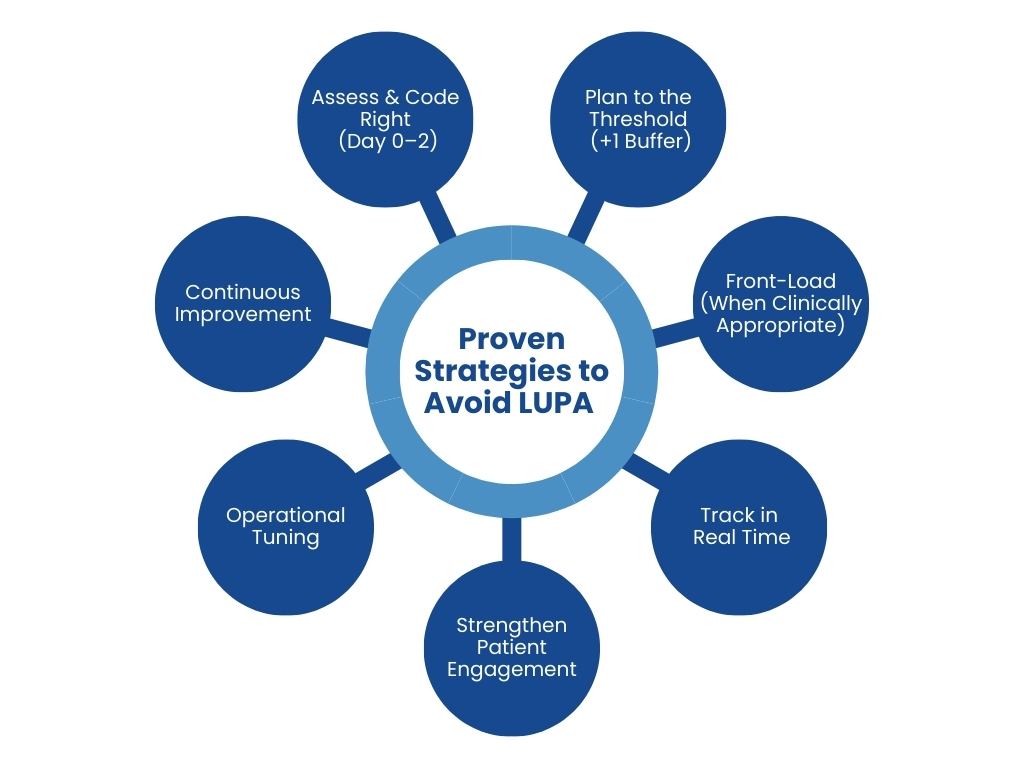
1. Assess & Code Right (Day 0–2)
Perfect the OASIS (especially M1800 functional items); inaccuracies here ripple into case-mix and thresholds.
Diagnosis precision: correct primary diagnosis for the clinical grouping; capture relevant comorbidities to reflect care complexity.
2. Plan to the Threshold (+1 Buffer)
- Translate the EMR’s lupa threshold into a concrete calendar plan.
- For low-visit cases, layer clinically appropriate supplemental touches (e.g., HH aide support, short check-in visits, RPM vitals review) to reinforce adherence and symptom management.
3. Front-Load (When Clinically Appropriate)
- Concentrate early, stabilizing visits in the first 10–14 days to reduce cancellations’ impact and improve outcomes.
4. Track in Real Time
- Daily review of “at-risk” episodes.
- Missed visit protocol: same-day outreach, reschedule within 72 hours when safe, and update the plan of care if patterns emerge.
5. Strengthen Patient Engagement
- Provide a visit calendar at SOC (start of care) and send reminders via SMS/phone.
- Use teach-back to confirm patients understand the importance of keeping early visits.
6. Operational Tuning
- Holiday coverage plans and cross-coverage for therapy disciplines.
- Float pool or per-diem coverage for weekends/peaks.
- Create time-window flexibility scripts to negotiate alternative slots with patients.
7. Continuous Improvement
- Monthly LUPA audit: categorize causes (refusals, staffing, documentation) and assign owners to fix.
- Refresh staff training based on audit findings; update scheduling templates and checklists.
Summary
LUPA doesn’t have to be a guessing game. When you understand what LUPA is, how PDGM sets each LUPA threshold, and the practical steps for LUPA compliance in home health care, you can protect reimbursement while delivering stronger, earlier interventions that patients feel. Build accurate OASIS and coding, plan visits to the threshold (+1 buffer), and track misses in real time; your revenue and outcomes will thank you. Want a head start? Download the simple LUPA threshold calculator and our pre-bill checklist to put this playbook into action today.